Heart failure afflicts more than 22 million people worldwide, and in the United States, is the most costly heart-related disease because of its chronicity (Collins, 2003). Failure of the left and/or right chambers of the heart results in insufficient output to meet tissue needs and causes pulmonary and systemic vascular congestion. Remodeling of the myocardium as a structural response to injury is one of the pathophysiologic causes of heart failure (HF). During remodeling the heart changes from an efficient football shape to an inefficient basketball shape, making coordinated contractility difficult. Despite diagnostic and therapeutic advances, HF continues to be associated with high morbidity and mortality. (Agency for Health Care Policy and Research [AHCPR] guidelines [6/94] promote the term heart failure [HF] in place of congestive heart failure [CHF] because many clients with heart failure do not manifest pulmonary or systemic congestion.) The New York Heart Association Functional Classification System for HF includes classes I– IV. Common causes of HF include ventricular dysfunction, cardiomyopathies, hypertension, coronary artery disease, valvular disease, and dysrhythmias.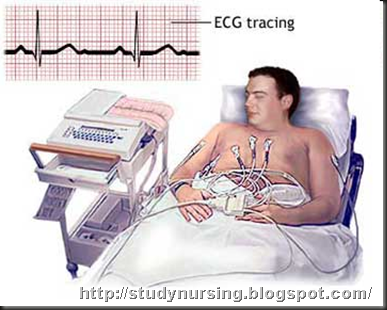
Care Setting
Although generally managed at the community level, inpatient stay may be required for periodic exacerbation of failure/development of complications.
Related Concerns
Myocardial infarction
Hypertension
Cardiac surgery
Dysrhythmias
Psychosocial aspects of care
Client Assessment Database
Activity/Rest
May report: Fatigue/exhaustion progressing throughout the day; exercise intolerance
Insomnia
Chest pain/pressure with activity
Dyspnea at rest or with exertion
May exhibit: Restlessness, mental status changes; e.g., anxiety and lethargy
Vital sign changes with activity
Circulation
May report: History of hypertension, recent/acute multiple MIs, previous episodes of HF, valvular heart disease, cardiac surgery, endocarditis, systemic lupus erythematosus (SLE), anemia, septic shock
Swelling of feet, legs, abdomen, “belt too tight” (right-sided heart failure)
May exhibit: BP may be low (pump failure), normal (mild or chronic HF), or high (fluid overload/increased systemic vascular resistance [SVR])
Pulse pressure may be narrow, reflecting reduced stroke volume
Tachycardia (may be left- or right-sided heart failure)
Dysrhythmias; e.g., atrial fibrillation, premature ventricular contractions/tachycardia, heart blocks
Apical pulse: PMI may be diffuse and displaced inferiorly to the left
Heart sounds: S3 (gallop) is diagnostic of congestive failure; S4 may occur; S1 and S2 may be softened
Systolic and diastolic murmurs may indicate the presence of valvular stenosis or insufficiency, both atrial and ventricular
Pulses: Peripheral pulses diminished; central pulses may be bounding; e.g., visible jugular, carotid, abdominal pulsations; alteration in strength of beat may be noted
Color ashen, pale, dusky, or even cyanotic
Nailbeds pale or cyanotic, with slow capillary refill
Liver may be enlarged/palpable, positive hepatojugular reflex
Breath sounds: Crackles, rhonchi
Edema may be dependent, generalized, or pitting, especially in extremities; JVD may be present
Ego Integrity
May report: Anxiety, apprehension, fear
Stress related to illness/financial concerns (job/cost of medical care)
May exhibit: Various behavioral manifestations; e.g., anxiety, anger, fear, irritability
Elimination
May report: Decreased voiding, dark urine
Night voiding (nocturia)
Diarrhea/constipation
Food/Fluid
May report: Loss of appetite/anorexia
Nausea/vomiting
Significant weight gain (may not respond to diuretic use)
Lower extremity swelling
Tight clothing/shoes
Diet high in salt/processed foods, fat, sugar, and caffeine
Use of diuretics
May exhibit: Rapid/continuous weight gain
Abdominal distention (ascites); edema (general, dependent, pitting, brawny)
Abdominal tenderness (ascites, hepatic engorgement)
Hygiene
May report: Fatigue/weakness, exhaustion during self-care activities
May exhibit: Appearance indicative of neglect of personal care
Neurosensory
May report: Weakness, dizziness, fainting episodes
May exhibit: Lethargy, confusion, disorientation
Behavior changes, irritability
Pain/Discomfort
May report: Chest pain, chronic or acute angina
Right upper abdominal pain (right-sided heart failure [RHF])
Generalized muscle aches/pains
May exhibit: Nervousness, restlessness
Narrowed focus (withdrawal)
Guarding behavior
Respiration
May report: Dyspnea on exertion, sleeping sitting up or with several pillows
Cough with/without sputum production, dry/hacking—especially when recumbent
History of chronic lung disease
Use of respiratory aids; e.g., oxygen and/or medications
May exhibit: Tachypnea; shallow, labored breathing; use of accessory muscles, nasal flaring
Cough: Dry/hacking/nonproductive or may be gurgling with/without sputum production
Sputum may be blood-tinged, pink/frothy (pulmonary edema)
Breath sounds may be diminished, with bibasilar crackles and wheezes
Mentation may be diminished; lethargy, restlessness present
Color: Pallor or cyanosis
Safety
May exhibit: Changes in mentation/confusion
Loss of strength/muscle tone
Skin excoriations, rashes
Social Interaction
May report: Decreased participation in usual social activities
Teaching/Learning
May report: Family history of developing HF at young age (genetic form). Family hisotry of heart disease, hypertension, diabetes (risk factors)
Use/misuse of cardiac medications; e.g., β-blockers, calcium channel blockers
Use of vitamins, herbal supplements (e.g., niacin, coenzyme Q10, garlic, ginkgo, black hellebore, dandelion), or aspirin
Recent/recurrent hospitalizations
Evidence of failure to improve
Discharge plan
considerations: Assistance with shopping, transportation, self-care needs, homemaker/maintenance tasks
Alteration in medication use/therapy
Changes in physical layout of home
Refer to section at end of plan for postdischarge considerations.
Diagnostic Studies
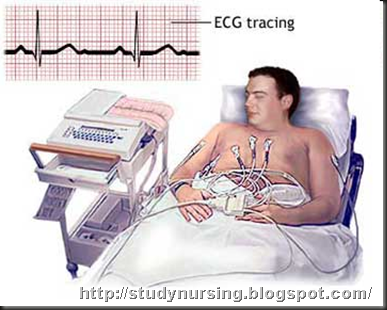
ECG: Ventricular or atrial hypertrophy, axis deviation, ischemia, and damage patterns may be present. Dysrhythmias; e.g., tachycardia, atrial fibrillation, conduction delays, especially left bundle branch block, frequent premature ventricular contractions (PVCs), may be present. Persistent ST-T segment abnormalities and decreased QRS amplitude may be present.
Chest x-ray: May show enlarged cardiac shadow, reflecting chamber dilatation/hypertrophy, or changes in blood vessels, reflecting increased pulmonary pressure. Abnormal contour; e.g., bulging of left cardiac border, may suggest ventricular aneurysm.
Sonograms (echocardiogram, Doppler and transesophageal echocardiogram): May reveal enlarged chamber dimensions, alterations in valvular function/structure, the degrees of ventricular dilation and dysfunction.
Heart scans:
Technetium-99m (99mTc) pyrophosphate scaning (also known as hot spot myocardial imaging and infarct avid imaging): Used to detect recent myocardial infaction and its extent.
Multigated acquisition (MUGA): Measures cardiac volume during both systole and diastole, measures ejection fraction, and estimates wall motion.
Exercise or pharmacologic stress myocardial perfusion (e.g., dipyridamole [Persantine] or thallium scan): Evaluates blood flow, determines presence of myocardial ischemia and wall motion abnormalities.
Positron emission tomography (PET) scan: Sensitive test for evaluation of myocardial ischemia/detecting viable myocardium.
Cardiac magnetic resonance imaging (MRI): Helps detect congenital heart disease, valvular heart disease, and vascular disorders such as thoracic aneurysm. It also helps detect cardiac tumors and structural anomalies.
Cardiac catheterization: Abnormal pressures are indicative of and help differentiate right-sided versus left-sided heart failure, as well as valve stenosis or insufficiency. Also assesses patency of coronary arteries. Contrast injected into the ventricles reveals abnormal size and ejection fraction/altered contractility. Transvenous endomyocardial biopsy may be useful in some clients to determine the underlying disorder, such as myocarditis or amylodosis.
BNP (Beta-type natruiretic peptide): Affects cardiac function and vascular tone and renal function. Low levels indicate worsening heart failure.
Liver enzymes: Elevated in liver congestion/failure.
Digoxin and other cardiac drug levels: Monitored to determine therapeutic range and correlate expected response with client response.
Bleeding and clotting times: Determine therapeutic range for anticoagulant therapy and/or identify those at risk for excessive clot formation.
Electrolytes: May be altered because of fluid shifts/decreased renal function and medications (e.g., diuretics, ACE inhibitors).
Arterial blood gases (ABGs): Left ventricular failure is characterized by mild respiratory alkalosis (early) or hypoxemia with an increased Pco2 (late).
BUN/creatinine: Elevated BUN suggests decreased renal perfusion as may occur with HF and/or as a side effect of prescribed medications (e.g., diuretics and ACE inhibitors). Elevation of both BUN and creatinine is indicative of renal failure.
Serum albumin/transferrin: May be decreased as a result of reduced protein intake or reduced protein synthesis in congested liver.
Complete blood count (CBC): May reveal anemia (major contributor/exacerbating factor in HF), polycythemia, or dilutional changes indicating water retention. Levels of white blood cells (WBCs) may be elevated, reflecting recent/acute MI, pericarditis, or other inflammatory or infectious states.
ESR: May be elevated, indicating acute inflammatory reaction (especially if viral infection is cause of HF).
Thyroid studies: Increased thyroid activity suggests thyroid hyperactivity as precipitator of HF. Hypothroydism can also cause or exacerbate HF.
Pulse oximetry: Oxygen saturation may be low, especially when acute HF is imposed on chronic obstructive pulmonary disease (COPD) or chronic HF.
Nursing Priorities
1. Improve myocardial contractility/systemic perfusion.
2. Reduce fluid volume overload.
3. Prevent complications.
4. Provide information about disease/prognosis, therapy needs, and prevention of recurrences.
Discharge Goals
1. Cardiac output adequate for individual needs.
2. Complications prevented/resolved.
3. Optimum level of activity/functioning attained.
4. Disease process/prognosis and therapeutic regimen understood.
5. Plan in place to meet needs after discharge.
NURSING DIAGNOSIS: decreased Cardiac Output
May be related to
Altered myocardial contractility/inotropic changes
Alterations in rate, rhythm, electrical conduction
Structural changes (e.g., valvular defects, ventricular aneurysm)
Possibly evidenced by
Increased heart rate (tachycardia), dysrhythmias, ECG changes
Changes in BP (hypotension/hypertension)
Extra heart sounds (S3, S4)
Decreased urine output
Diminished peripheral pulses
Cool, ashen skin; diaphoresis
Orthopnea, crackles, JVD, liver engorgement, edema
Chest pain
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Cardiac Pump Effectiveness (NOC)
Display vital signs within acceptable limits, dysrhythmias absent/controlled, and no symptoms of failure (e.g., hemodynamic parameters within acceptable limits, urinary output adequate).
Report decreased episodes of dyspnea, angina.
Cardiac Disease Self-Management (NOC)
Participate in activities that reduce cardiac workload.
| ACTIONS/INTERVENTIONS Hemodynamic Regulation (NIC)
Independent - Auscultate apical pulse; assess heart rate, rhythm (document dysrhythmia if telemetry available).
- Note heart sounds.
| RATIONALE
- Tachycardia is usually present (even at rest) to compensate for decreased ventricular contractility. Premature atrial contractions (PACs), paroxysmal atrial tachycardia (PAT), PVCs, multifocal atrial tachycardia (MAT), and atrial fibrillation (AF) are common dysrhythmias associated with HF, although others may also occur. Note: Intractable ventricular dysrhythmias unresponsive to medication suggest ventricular aneurysm.
- S1 and S2 may be weak because of diminished pumping action. Gallop rhythms are common (S3 and S4), produced as blood flows into noncompliant/distended chambers. Murmurs may reflect valvular incompetence/stenosis.
|
- Palpate peripheral pulses.
- Monitor BP.
- Inspect skin for pallor, cyanosis.
- Monitor urine output, noting decreasing output and dark/concentrated urine.
- Note changes in sensorium; e.g., lethargy, confusion, disorientation, anxiety, and depression.
- Encourage rest, semirecumbent in bed or chair. Assist with physical care as indicated.
- Provide quiet environment; explain medical/nursing management; help client avoid stressful situations; listen/respond to expressions of feelings/fears.
- Provide bedside commode. Have client avoid activities eliciting a vasovagal response; e.g., straining during defecation, holding breath during position changes.
- Elevate legs, avoiding pressure under knee. Encourage active/passive exercises. Increase ambulation/activity as tolerated.
- Check for calf tenderness; diminished pedal pulse; swelling, local redness, or pallor of extremity.
- Withhold digitalis preparation as indicated, and notify physician if marked changes occur in cardiac rate or rhythm or signs of digitalis toxicity occur.
- CollaborativeAdminister supplemental oxygen as indicated.
- Administer medications as indicated:
- Diuretics, e.g., furosemide (Lasix), ethacrynic acid (Edecrin), bumetanide (Bumex), spironolactone (Aldactone);
- Vasodilators, e.g., nitrates (Nitro-Dur, Isordil); arteriodilators; e.g., hydralazine (Apresoline); combination drugs; e.g., prazosin (Minipress); nesiritide (Natrecor);
- ACE inhibitors; e.g., benazepril (Lotensin), captopril (Capoten), lisinopril (Prinivil), enalapril (Vasotec), quinapril (Accupril), ramipril (Altace), moexipril (Univasc);
- Angiotensin II receptor antagonists, (also known as angiotension receptor blockers [ARBs]); e.g., candesartan (Atacand), losartan (Cozaar), eprosartan (Teveten), ibesartan (Avapro), valsartan (Diovan);
- Digoxin (Lanoxin);
- Inotropic agents; e.g., amrinone (Inocor), milrinone (Primacor), vesnarinone (Arkin-Z);
- β-adrenergic receptor antagonists; e.g., carvedilol (Coreg), bisoprolol (Zebeta), metoprolol (Lopressor);
- Aldosterone antagonist; e.g. eplerenone (Inspra);
- Morphine sulfate;
- Antianxiety agents/sedatives;
| - Decreased cardiac output may be reflected in diminished radial, popliteal, dorsalis pedis, and posttibial pulses. Pulses may be fleeting or irregular to palpation, and pulsus alternans (strong beat alternating with weak beat) may be present.
- In early, moderate, or chronic HF, BP may be elevated because of increased SVR. In advanced HF, the body may no longer be able to compensate, and profound/irreversible hypotension may occur.
- Pallor is indicative of diminished peripheral perfusion secondary to inadequate cardiac output, vasoconstriction, and anemia. Cyanosis may develop in refractory HF. Dependent areas are often blue or mottled as venous congestion increases.
- Kidneys respond to reduced cardiac output by retaining water and sodium. Urine output is usually decreased during the day because of fluid shifts into tissues but may be increased at night because fluid returns to circulation when client is recumbent.
- May indicate inadequate cerebral perfusion secondary to decreased cardiac output.
- Physical rest should be maintained during acute or refractory HF to improve efficiency of cardiac contraction and to decrease myocardial oxygen demand/consumption and workload.
- Psychologic rest helps reduce emotional stress, which can produce vasoconstriction, elevating BP and increasing heart rate/work.
- Commode use decreases work of getting to bathroom or struggling to use bedpan. Vasovagal maneuver causes vagal stimulation followed by rebound tachycardia, which further compromises cardiac function/output.
- Decreases venous stasis, and may reduce incidence of thrombus/embolus formation.
- Reduced cardiac output, venous pooling/stasis, and enforced bed rest increases risk of thrombophlebitis.
- Incidence of toxicity is high (20%) because of narrow margin between therapeutic and toxic ranges. Digoxin may have to be discontinued in the presence of toxic drug levels, a slow heart rate, or low potassium level. (Refer to CP: Dysrhythmias; ND: risk for Poisoning: digitalis toxicity.[KMcC1] )
- Increases available oxygen for myocardial uptake to combat effects of hypoxia/ischemia.
- A variety of medications may be used to increase stroke volume, improve contractility, and reduce congestion.
- Diuretics, in conjunction with restriction of dietary sodium and fluids, often lead to clinical improvement in clients with stages I and II HF. In general, type and dosage of diuretic depend on cause and degree of HF and state of renal function. Preload reduction is most useful in treating clients with a relatively normal cardiac output accompanied by congestive symptoms. Loop diuretics block chloride reabsorption, thus interfering with the reabsorption of sodium and water.
- Vasodilators are the mainstay of treatment in HF and are used to increase cardiac and renal output, reducing circulating volume (preload and afterload) and decreasing SVR, thereby reducing ventricular workload. Note: Nesiritide is used in acutely decompensated CHF and has been used with digoxin, diuretics, and ACE inhibitors. Parenteral vasodilators are reserved for clients with severe HF or those unable to take oral medications.
- ACE inhibitors represent first-line therapy to control heart failure by decreasing venticular filling pressures and SVR while increasing cardiac output with little or no change in BP and heart rate.
- Antihypertensive and cardioprotective effects are attributable to selective blockade of AT1 (angiotensin II) receptors and angiotensin II synthesis. Note: ARBs used in combination with ACE inhibitors and β-blockers are thought to have decreased hospitalizations for HF clients.
- Increases force of myocardial contraction when diminished contractility is the cause of HF, and slows heart rate by decreasing conduction velocity and prolonging refractory period of the atrioventricular (AV) junction to increase cardiac efficiency/output.
- These medications are useful for short-term treatment of HF unresponsive to cardiac glycosides, vasodilators, and diuretics in order to increase myocardial contractility and produce vasodilation. Positive inotropic properties have reduced mortality rates 50% and improved quality of life.
- Useful in the treatment of HF by blocking the cardiac effects of chronic adrenergic stimulation. Many clients experience improved activity tolerance and ejection fraction.
- Approved by the Food and Drug Administration (FDA) in 2003, eplerenone has been shown to improve survival in HF, especially following MI.
- Decreases vascular resistance and venous return, reducing myocardial workload, especially when pulmonary congestion is present. Allays anxiety and breaks the feedback cycle of anxiety to catecholamine release to anxiety.
- Promote rest/relaxation, reducing oxygen demand and myocardial workload.
|
- Anticoagulants; e.g., low-dose heparin, warfarin (Coumadin).
- Administer IV solutions, restricting total amount as indicated. Avoid saline solutions.
- Monitor/replace electrolytes.
- Monitor serial ECG and chest x-ray changes.
- Measure cardiac output and other functional parameters as indicated.
- Monitor laboratory studies; e.g., BUN, creatinine:
- Liver function studies (AST, LDH);
- Prothrombin time (PT)/activated partial thromboplastin time (aPTT) coagulation studies.
- Prepare for insertion/maintain pacemaker(or pacemaker/defibrillator), if indicated.
- Prepare for surgery as indicated; e.g., valve replacement, angioplasty, coronary artery bypass grafting (CABG);
| - May be used prophylactically to prevent thrombus/embolus formation in the presence of risk factors such as venous stasis, enforced bedrest, cardiac dysrhythmias, and history of previous thrombolic episodes.
- Because of existing elevated left ventricular pressure, client may not tolerate increased fluid volume (preload). Clients with HF also excrete less sodium, which causes fluid retention and increases myocardial workload.
- Fluid shifts and use of diuretics can alter electrolytes (especially potassium and chloride), which affect cardiac rhythm and contractility.
- ST segment depression and T wave flattening can develop because of increased myocardial oxygen demand, even if no coronary artery disease is present. Chest x-ray may show enlarged heart and changes of pulmonary congestion.
- Cardiac index, preload/afterload, contractility, and cardiac work can be measured noninvasively by using thoracic electrical bioimpedance (TEB) technique. Useful in determining effectiveness of therapeutic interventions and response to activity.
- Elevation of BUN/creatinine reflects kidney hypoperfusion/failure.
- May be elevated because of liver congestion and indicate need for smaller dosages of medications that are detoxified by the liver.
- Measures changes in coagulation processes or effectiveness of anticoagulant therapy.
- May be necessary to correct bradydysrhythmias unresponsive to drug intervention, which can aggravate congestive failure/produce pulmonary edema. Note: Beiventricular pacemaker and cardiac defibirillators are designed to provide resynchronization for the heart by simultaneous electrical activation of both the right and left sides of the heart, thereby creating a more effective and efficient pump.
- Heart failure due to ventricular aneurysm or valvular dysfunction may require aneurysmectomy or valve replacement to improve myocardial contractility/ function. Revascularization of cardiac muscle by CABG may be done to improve cardiac function.
|
- Cardiomyoplasty;
- Transmyocardial revascularization.
- Assist with/maintain mechanical circulatory support system, such as IABP or LVAD, when indicated.
| - Cardiomyoplasty, an experimental procedure in which the latissimus dorsi muscle is wrapped around the heart and electrically stimulated to contract with each heartbeat, may be done to augment ventricular function while the client is awaiting cardiac transplantation or when transplantation is not an option.
- Other new surgical techniques include transmyocardial revascularization (percutaneous [PTMR]) using CO2 laser technology, in which a laser is used to create multiple 1-mm diameter channels in viable but underperfused cardiac muscle.
- An intra-aortic balloon pump (IABP) may be inserted as a temporary support to the failing heart in the critically ill client with potentially reversible HF. A battery-powered left-ventricular assist device (LVAD) may also be used positioned between the cardiac apex and the descending thoracic or abdominal aorta. This device receives blood from the left ventricle (LV) and ejects it into the systemic circulation, often allowing client to resume a nearly normal lifestyle while awaiting heart transplantation, or in some instances, allows the heart to recover and regain its function.. With end-stage HF, cardiac transplantation may be indicated.
|
NURSING DIAGNOSIS: Activity Intolerance
May be related to
Imbalance between oxygen supply/demand
Generalized weakness
Prolonged bedrest/immobility
Possibly evidenced by
Weakness, fatigue
Changes in vital signs, presence of dysrhythmias
Dyspnea
Pallor, diaphoresis
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Endurance (NOC)
Participate in desired activities; meet own self-care needs.
Achieve measurable increase in activity tolerance, evidenced by reduced fatigue and weakness and by vital signs within acceptable limits during activity.
| ACTIONS/INTERVENTIONS Energy Management (NIC)
Independent
- Check vital signs before and immediately after activity, especially if client is receiving vasodilators, diuretics, or β-blockers.
- Document cardiopulmonary response to activity. Note tachycardia, dysrhythmias, dyspnea, diaphoresis, pallor.
- Assess for other precipitators/causes of fatigue; e.g., treatments, pain, medications.
- Evaluate accelerating activity intolerance.
- Provide assistance with self-care activities as indicated. Intersperse activity periods with rest periods.
Collaborative
- Implement graded cardiac rehabilitation/activity program.
| RATIONALE
- Orthostatic hypotension can occur with activity because of medication effect (vasodilation), fluid shifts (diuresis), or compromised cardiac pumping function.
- Compromised myocardium/inability to increase stroke volume during activity may cause an immediate increase in heart rate and oxygen demands, thereby aggravating weakness and fatigue.
- Fatigue is a side effect of some medications (e.g., β-blockers, tranquilizers, and sedatives). Pain and stressful regimens also extract energy and produce fatigue.
- May denote increasing cardiac decompensation rather than overactivity.
- Meets client’s personal care needs without undue myocardial stress/excessive oxygen demand.
- Strengthens and improves cardiac function under stress if cardiac dysfunction is not irreversible. Gradual increase in activity avoids excessive myocardial workload and oxygen consumption.
|
NURSING DIAGNOSIS: excess Fluid Volume
May be related to
Reduced glomerular filtration rate (decreased cardiac output)/increased antidiuretic hormone (ADH) production, and sodium/water retention
Possibly evidenced by
Orthopnea, S3 heart sound
Oliguria, edema, JVD, positive hepatojugular reflex
Weight gain
Hypertension
Respiratory distress, abnormal breath sounds
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Fluid Balance (NOC)
Demonstrate stabilized fluid volume with balanced intake and output, breath sounds clear/clearing, vital signs within acceptable range, stable weight, and absence of edema.
Verbalize understanding of individual dietary/fluid restrictions.
| ACTIONS/INTERVENTIONS Fluid Management (NIC) Independent
- Monitor urine output, noting amount and color, as well as time of day when diuresis occurs.
- Monitor/calculate 24-hour intake and output (I&O) balance.
- Maintain chair or bed rest in semi-Fowler’s position during acute phase.
- Establish fluid intake schedule if fluids are medically restricted, incorporating beverage preferences when possible. Give frequent mouth care/ice chips as part of fluid allotment.
- Weigh daily.
- Assess for distended neck and peripheral vessels. Inspect dependent body areas for edema with/without pitting; note presence of generalized body edema (anasarca).
- Change position frequently. Elevate feet when sitting. Inspect skin surface, keep dry, and provide padding as indicated. (Refer to ND: risk for impaired Skin Integrity.)
- Auscultate breath sounds, noting decreased and/or adventitious sounds; e.g., crackles, wheezes. Note presence of increased dyspnea, tachypnea, orthopnea, paroxysmal nocturnal dyspnea, persistent cough.
- Investigate reports of sudden extreme dyspnea/air hunger, need to sit straight up, sensation of suffocation, feelings of panic or impending doom.
- Monitor BP and central venous pressure (CVP) (if available).
| RATIONALE - Urine output may be scanty and concentrated (especially during the day) because of reduced renal perfusion. Recumbency favors diuresis; therefore, urine output may be increased at night/during bedrest.
- Diuretic therapy may result in sudden/excessive fluid loss (circulating hypovolemia), even though edema/ascites remains.
- Recumbency increases glomerular filtration and decreases production of ADH, thereby enhancing diuresis.
- Involving client in therapy regimen may enhance sense of control and cooperation with restrictions.
- Documents changes in/resolution of edema in response to therapy. A gain of 5 lb represents approximately 2 L of fluid. Conversely, diuretics can result in rapid/excessive fluid shifts and weight loss.
- Excessive fluid retention may be manifested by venous engorgement and edema formation. Peripheral edema begins in feet/ankles (or dependent areas) and ascends as failure worsens. Pitting edema is generally obvious only after retention of at least 10 lb of fluid. Increased vascular congestion (associated with RHF) eventually results in systemic tissue edema.
- Edema formation, slowed circulation, altered nutritional intake, and prolonged immobility/bedrest are cumulative stressors that affect skin integrity and require close supervision/preventive interventions.
- Excess fluid volume often leads to pulmonary congestion. Symptoms of pulmonary edema may reflect acute left-sided HF. RHF’s respiratory symptoms (dyspnea, cough, orthopnea) may have slower onset but are more difficult to reverse.
- May indicate development of complications (pulmonary edema/embolus) and differs from orthopnea paroxysmal nocturnal dyspnea in that it develops much more rapidly and requires immediate intervention.
- Hypertension and elevated CVP suggest fluid volume excess and may reflect developing/increasing pulmonary congestion, HF.
|
- Assess bowel sounds. Note complaints of anorexia, nausea, abdominal distention, constipation.
- Provide small, frequent, easily digestible meals.
- Measure abdominal girth, as indicated.
- Encourage verbalization of feelings regarding limitations.
- Palpate abdomen. Note reports of right upper quadrant pain/tenderness.
- Note increased lethargy, hypotension, muscle cramping.
Collaborative Fluid/Electolyte Management (NIC)
Administer medications as indicated: - Diuretics; e.g., furosemide (Lasix), bumetanide (Bumex);Thiazides with potassium-sparing agents; e.g., spironolactone (Aldactone);
- Potassium supplements; e.g., K-Dur.
- Maintain fluid/sodium restrictions as indicated.
- Consult with dietitian.
- Monitor chest x-ray.
- Assist with rotating tourniquets/phlebotomy, dialysis, or ultrafiltration as indicated.
| - Visceral congestion (occurring in progressive HF) can alter gastric/intestinal function.
- Reduced gastric motility can adversely affect digestion and absorption. Small, frequent meals may enhance digestion/prevent abdominal discomfort.
- In progressive RHF, fluid may shift into the peritoneal space, causing increasing abdominal girth (ascites).
- Expression of feelings/concerns may decrease stress/anxiety, which is an energy drain that can contribute to feelings of fatigue.
- Advancing HF leads to venous congestion, resulting in abdominal distention, liver engorgement (hepatomegaly), and pain. This can alter liver function and impair/prolong drug metabolism.
- Signs of potassium and sodium deficits that may occur because of fluid shifts and diuretic therapy.
- Increases rate of urine flow and may inhibit reabsorption of sodium/chloride in the renal tubules.
- Promotes diuresis without excessive potassium losses.
- Replaces potassium that is lost as a common side effect of diuretic therapy, which can adversely affect cardiac function.
- Reduces total body water/prevents fluid reaccumulation.
- May be necessary to provide diet acceptable to client that meets caloric needs within sodium restriction.
- Reveals changes indicative of increase/resolution of pulmonary congestion.
- Although not frequently used, mechanical fluid removal rapidly reduces circulating volume, especially in pulmonary edema refractory to other therapies.
|
NURSING DIAGNOSIS: risk for impaired Gas Exchange
Risk factors may include
Alveolar-capillary membrane changes; e.g., fluid collection/shifts into interstitial space/alveoli
Possibly evidenced by
[Not applicable; presence of signs and symptoms establishes an actual diagnosis.]
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Respiratory Status: Gas Exchange (NOC)
Demonstrate adequate ventilation and oxygenation of tissues by ABGs/oximetry within client’s normal ranges and free of symptoms of respiratory distress.
Participate in treatment regimen within level of ability/situation.
| ACTIONS/INTERVENTIONS Airway Management (NIC)
Independent
- Auscultate breath sounds, noting crackles, wheezes.
- Instruct client in effective coughing, deep breathing.
- Encourage frequent position changes.
- Maintain chair/bedrest with head of bed elevated 20–30 degrees, semi-Fowler’s position. Support arms with pillows.
Collaborative
- Monitor/graph serial ABGs, pulse oximetry.
- Administer supplemental oxygen as indicated.
- Administer medications as indicated:Diuretics; e.g., furosemide (Lasix);
- Bronchodilators; e.g., aminophylline.
| RATIONALE
- Reveals presence of pulmonary congestion/collection of secretions, indicating need for further intervention.
- Clears airways and facilitates oxygen delivery.
- Helps prevent atelectasis and pneumonia.
- Reduces oxygen consumption/demands and promotes maximal lung inflation.
- Hypoxemia can be severe during pulmonary edema. Compensatory changes are usually present in chronic HF. Note: In clients with abnormal cardiac index, research suggests pulse oximeter measurements may exceed actual oxygen saturation by up to 7%.
- Increases alveolar oxygen concentration, which may correct/reduce tissue hypoxemia.
- Reduces alveolar congestion, enhancing gas exchange.
- Increases oxygen delivery by dilating small airways, and exerts mild diuretic effect to aid in reducing pulmonary congestion.
|
NURSING DIAGNOSIS: risk for impaired Skin Integrity
Risk factors may include
Prolonged bedrest
Edema, decreased tissue perfusion
Possibly evidenced by
[Not applicable; presence of signs and symptoms establishes an actual diagnosis.]
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Tissue Perfusion: Peripheral (NOC)
Maintain skin integrity.
Demonstrate behaviors/techniques to prevent skin breakdown.
| ACTIONS/INTERVENTIONS Pressure Management (NIC)
Independent
- Inspect skin, noting skeletal prominences, presence of edema, areas of altered circulation/pigmentation, or obesity/emaciation.
- Provide gentle massage around reddened or blanched areas.
- Encourage frequent position changes in bed/chair, assist with active/passive range of motion (ROM) exercises.
- Provide frequent skin care; minimize contact with moisture/excretions.
- Check fit of shoes/slippers and change as needed.
- Avoid intramuscular route for medication administration.
Collaborative
- Provide alternating pressure/egg-crate mattress, sheepskin elbow/heel protectors.
| RATIONALE
- Skin is at risk because of impaired peripheral circulation, physical immobility, and alterations in nutritional status.
- Improves blood flow, minimizing tissue hypoxia. Note: Direct massage of compromised area may cause tissue injury.
- Reduces pressure on tissues, improving circulation and reducing time any one area is deprived of full blood flow.
- Excessive dryness or moisture damages skin and hastens breakdown.
- Dependent edema may cause shoes to fit poorly, increasing risk of pressure and skin breakdown on feet.
- Interstitial edema and impaired circulation impede drug absorption and predispose to tissue breakdown/development of infection.
- Reduces pressure to skin, may improve circulation.
|
NURSING DIAGNOSIS: deficient Knowledge (Learning Need] regarding condition, treatment regimen, self-care, and discharge needs
May be related to
Lack of understanding/misconceptions about interrelatedness of cardiac function/disease/failure
Possibly evidenced by
Questions
Statements of concern/misconceptions
Recurrent, preventable episodes of HF
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Knowledge: Cardiac Disease Management (NOC)
Identify relationship of ongoing therapies (treatment program) to reduction of recurrent episodes and prevention of complications.
List signs/symptoms that require immediate intervention.
Identify own stress/risk factors and some techniques for handling.
Initiate necessary lifestyle/behavioral changes.
| ACTIONS/INTERVENTIONS Teaching: Disease Process (NIC)
Independent
- Discuss normal heart function. Include information regarding client’s variance from normal function. Explain difference between heart attack and HF.
- Reinforce treatment rationale. Include significant other (SO)/family members in teaching as appropriate, especially for complicated regimens such as management of technology (e.g., implantable cardioverter defibrillator [ICD], left vetricular assist device [LVAD]), or dobutamine infusion home therapy when client does not respond to customary combination therapy or cannot be weaned from dobutamine, or those awaiting heart transplant.
- Encourage developing a regular home exercise program, and provide guidelines for sexual activity.
- Discuss importance of being as active as possible without becoming exhausted and need for rest between activities.
| RATIONALE - Knowledge of disease process and expectations can facilitate adherence to prescribed treatment regimen.
- Client may believe it is acceptable to alter postdischarge regimen when feeling well and symptom-free or when feeling below par, which can increase the risk of exacerbation of symptoms. Understanding of regimen, medications, tehcnology , and restrictions may augment cooperation with control of symptoms. Home IV therapy requires a significant commitment by caregivers to operate/troubleshoot infusion pump, change dressing for peripherally inserted central catheter (PICC) line, and monitor I&O and signs/symptoms of HF.
- Promotes maintenance of muscle tone and organ function for overall sense of well-being. Changing sexual habits (e.g., sex in morning when well rested, client on top, inclusion of other physical expressions of affection) may be difficult but provides opportunity for continuing satisfying sexual relationship.
- Excessive physical activity or overexertion can further weaken the heart, exacerbating failure, and necessitates adjustment of exercise program.
|
- Discuss importance of sodium limitation. Provide list of sodium content of common foods that are to be avoided/limited. Encourage reading of labels on food and drug packages.
- Refer to dietitian for counseling specific to individual needs/dietary customs.
- Review medications, purpose, and side effects. Provide both oral and written instructions.
- Recommend taking diuretic early in morning.
- Instruct and receive return demonstration of ability to take and record daily pulse and blood pressure and when to notify healthcare provider; e.g., parameters above/below preset rate, changes in rhythm/regularity.
- Explain and discuss client’s role in control of risk factors (e.g., smoking) and precipitating or aggravating factors (e.g., high-salt diet, inactivity/overexertion, exposure to extremes in temperature).
- Review signs/symptoms that require immediate medical attention; e.g., rapid/significant weight gain, edema, shortness of breath, increased fatigue, cough, hemoptysis, fever.
- Provide opportunities for client/SO to ask questions, discuss concerns, and make necessary lifestyle changes.
| - Dietary intake of sodium of more than 3 g/day can offset effect of diuretic. Most common source of sodium is table salt and obviously salty foods, although canned soups/vegetables, luncheon meats, and dairy products also may contain high levels of sodium.
- Identifies dietary needs, especially in presence of obesity (major risk factor for developing HF), diabetes, or presence of nausea/vomiting and resulting wasting syndrome (cardiac cachexia). Eating six small meals and using liquid dietary supplements and vitamin supplements can limit inappropriate weight loss.
- Understanding therapeutic needs and importance of prompt reporting of side effects can prevent occurrence of drug-related complications. Anxiety may block comprehension of input or details, and client/SO may refer to written material at later date to refresh memory.
- Provides adequate time for drug effect before bedtime to prevent/limit interruption of sleep.
- Promotes self-monitoring of condition/drug effect. Early detection of changes allows for timely intervention and may prevent complications, such as digitalis toxicity.
- Adds to body of knowledge, and permits client to make informed decisions regarding control of condition and prevention of recurrence/complications. Smoking potentiates vasoconstriction; sodium intake promotes water retention/edema formation; improper balance between activity and rest and exposure to temperature extremes may result in exhaustion/increased myocardial workload and increased risk of respiratory infections. Alcohol can depress cardiac contractility. Limitation of alcohol use to social occasions or maximum of one drink/day may be tolerated unless cardiomyopathy is alcohol induced (requiring complete abstinence).
- Self-monitoring increases client responsibility in health maintenance and aids in prevention of complications; e.g., pulmonary edema, pneumonia. Weight gain of more than 3 lb in a week requires medical evaluation/adjustment of diuretic therapy. Note: Client should weigh self daily in morning without clothing, after voiding and before eating.
- Chronicity and recurrent/debilitating nature of HF often exhausts coping abilities and supportive capacity of both client and SO, leading to depression.
|
- Discuss general health risks (such as infection), recommending avoidance of crowds and individuals with respiratory infections, obtaining yearly influenza immunization and one-time pneumonia immunization.
- Stress importance of reporting signs/symptoms of digitalis toxicity; e.g., development of gastrointestinal (GI) and visual disturbances, changes in pulse rate/rhythm, worsening of heart failure.
- Identify community resources/support groups and visiting home health nurse as indicated.
- Discuss importance of advance directives and of communicating plan/wishes to family and primary care providers.
| - This population is at increased risk for infection because of circulatory compromise.
- Early recognition of developing complications and involvement of healthcare provider may prevent toxicity/hospitalization.
- May need additional assistance with self-monitoring/home management, especially when HF is progressive.
- Up to 50% of all deaths from heart failure are sudden, with many occurring at home, possibly without significant worsening of symptoms. If client chooses to refuse life-support measures, an alternative contact person (rather than 911) needs to be designated, should cardiac arrest occur.
|
POTENTIAL CONSIDERATIONS following discharge from care setting (dependent on client’s age, physical condition/presence of complications, personal resources, and life responsibilities)
Activity Intolerance—poor cardiac reserve, side effects of medication, generalized weakness.
excess or deficient Fluid Volume—changes in glomerular filtration rate, diuretic use, individual fluid/salt intake.
impaired Skin Integrity—decreased activity level, prolonged sitting, presence of edema, altered circulation.
ineffective Therapeutic Regimen Management—complexity of regimen, economic limitations.
impaired Home Maintenance—chronic/debilitating condition, insufficient finances, inadequate support systems.
Self-Care Deficit—decreased strength/endurance, depression.
No comments:
Post a Comment