A bronchography is a radiographic (x-ray) examination of the interior passageways of the lower respiratory tract. The structures of the lower respiratory tract, which include the larynx (voice box), trachea (windpipe), and bronchi (larger branching airways to the lungs), become visible on x-ray film after contrast dye is instilled through either a catheter or bronchoscope (narrow, flexible, lighted tube) into these areas. Contrast dye is a substance that causes a particular organ, tissue, or structure to be more visible on x-ray or other diagnostic images.
The contrast dye is released as the catheter or bronchoscope is inserted through the nose or mouth and advanced down the throat into the trachea and bronchi. The contrast dye forms a coating on the lining of the interior walls of these structures, thus outlining their anatomy on x-ray. In addition, abnormalities such as tumors, cavities, cysts, and obstructions may be revealed.
As a result of improved computerized tomography (CT scan) and bronchoscopy technology, as well as increased availability of these procedures, bronchography is performed on an infrequent basis.
Other related procedures that may be used to diagnose problems of the lungs and respiratory tract include bronchoscopy, CT scan of the chest, chest fluoroscopy, chest x-ray, chest ultrasound, lung biopsy, lung scan, mediastinoscopy, oximetry, peak flow measurement, positron emission tomography (PET) scan, pulmonary angiogram, pulmonary function tests, and thoracentesis. Please see these procedures for additional information.
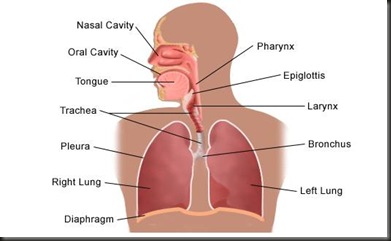
Anatomy of the respiratory system:
The respiratory system is made up of the organs involved in the interchanges of gases, and consists of the:
- nose
- pharynx
- larynx
- trachea
- bronchi
- lungs
The upper respiratory tract includes the:
- nose
- nasal cavity
- ethmoidal air cells
- frontal sinuses
- maxillary sinus
- larynx
- trachea
The lower respiratory tract includes the lungs, bronchi, and alveoli.
What are the functions of the lungs?
The lungs take in oxygen, which cells need to live and carry out their normal functions. The lungs also get rid of carbon dioxide, a waste product of the body's cells.
The lungs are a pair of cone-shaped organs made up of spongy, pinkish-gray tissue. They take up most of the space in the chest, or the thorax (the part of the body between the base of the neck and diaphragm).
The lungs are enveloped in a membrane called the pleura.
The lungs are separated from each other by the mediastinum, an area that contains the following:
- the heart and its large vessels
- trachea (windpipe)
- esophagus
- thymus
- lymph nodes
The right lung has three sections, called lobes. The left lung has two lobes. When you breathe, the air enters the body through the nose or the mouth. It then travels down the throat through the larynx (voice box) and trachea (windpipe) and goes into the lungs through tubes called main-stem bronchi.
One main-stem bronchus leads to the right lung and one to the left lung. In the lungs, the main-stem bronchi divide into smaller bronchi and then into even smaller tubes called bronchioles. Bronchioles end in tiny air sacs called alveoli.
A bronchography may be performed to diagnose structural or functional abnormalities of the larynx, trachea, and/or bronchi. Abnormalities may include, but are not limited to, the following:
- bronchiectasis - an irreversible enlargement of the bronchi as a result of deterioration of the muscle and elastic tissue of the bronchial walls. Generally, this is the result of chronic inflammation from various causes.
- hemoptysis - coughing up blood
- tracheoesophageal fistula - abnormal tract between trachea (windpipe) and esophagus (hollow tube used for swallowing)
- tumors (abnormal growths)
- chronic pneumonia or bronchitis
There may be other reasons for your physician to recommend a bronchography.
As with any invasive procedure, complications may occur. Complications related to bronchography may include, but are not limited to, the following:
- infection or pneumonia
- airway obstruction from the contrast dye in patients with emphysema or chronic bronchitis
- bronchospasm or laryngospasm from the contrast dye in patients with asthma
You may want to ask your physician about the amount of radiation used during the procedure and the risks related to your particular situation. It is a good idea to keep a record of your past history of radiation exposure, such as previous scans and other types of x-rays, so that you can inform your physician. Risks associated with radiation exposure may be related to the cumulative number of x-ray examinations and/or treatments over a long period of time.
If you are pregnant or suspect that you may be pregnant, you should notify your physician. Radiation exposure during pregnancy may lead to birth defects.
Patients who are allergic to or sensitive to medications, contrast dyes, iodine, shellfish, or latex should notify their physician.
Contraindications for bronchography may include pregnancy, a productive cough, acute respiratory infection, and respiratory insufficiency.
There may be other risks depending upon your specific medical condition. Be sure to discuss any concerns with your physician prior to the procedure.
Coughing and/or sputum in the airways may interfere with a bronchography.
- Your physician will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- Notify your physician if you are allergic to or sensitive to medications, local and general anesthesia, contrast dyes, iodine, shellfish, or latex.
- You will be asked to fast for a certain period of time before the procedure. Your physician will notify you how long to fast, whether for a few hours or overnight.
- If you are pregnant or suspect that you may be pregnant, you should notify your physician.
- Notify your physician of all medications (prescription and over-the-counter) and herbal supplements that you are taking.
- Notify your physician if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
- You may be asked to perform thorough mouth hygiene prior to the procedure.
- If a sedative is given before the procedure, you may need someone to drive you home afterwards. If the procedure is to be done under general anesthesia, you will receive a sedative prior to the procedure.
- Based upon your medical condition, your physician may request other specific preparation.
A bronchography may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your physician’s practices.
Generally, a bronchography follows this process:
- You will be asked to remove any clothing, jewelry, dentures, or other objects that may interfere with the procedure.
- If you are asked to remove clothing, you will be given a gown to wear.
- You will be asked to empty your bladder prior to the procedure.
- An intravenous (IV) line may be inserted in your arm or hand.
- Your heart rate, blood pressure, respiratory rate, and oxygen level may be monitored during the procedure.
- You will be positioned sitting upright on a table that can tilt you from a horizontal to an upright position as well as other positions. Changing positions aids in the distribution of the contrast dye into different areas for examination.
- You may be given a sedative to make you sleepy but arousable.
- Numbing medication will be sprayed into the back of your throat to prevent gagging as the bronchoscope is passed down your throat into your stomach. The spray may have a bitter taste to it. Holding your breath while the physician sprays your throat may decrease the taste.
- You will not be able to swallow the saliva that may collect in your mouth during the procedure due to the bronchoscope in your throat. The saliva will be suctioned from your mouth from time to time.
- The physician will pass the catheter or bronchoscope down the back of the throat into the trachea and the bronchus, instilling the contrast dye as the instrument is advanced.
- You may experience some discomfort when the catheter or bronchoscope is advanced. Your airway will not be blocked.
- Your physician will take several x-rays in various positions.
- Once all required x-rays have been taken, the catheter or bronchoscope will be removed.
After the procedure, you will be taken to the recovery room for observation. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged to your home. If this procedure was performed on an outpatient basis, you should plan to have another person drive you home.
You will not be allowed to eat or drink anything until your gag reflex has returned. You may notice some soreness of your throat and pain with swallowing for a few days. This soreness is normal.
You may be instructed to gently cough up and spit any remaining contrast dye into a basin to aid in clearing your airways. The physician may recommend postural drainage (lying flat with the head lower than the rest of the body while the physician or nurse gently pats your back to help drain the secretions).
You may resume your usual diet after the procedure, unless your physician decides otherwise. You may be advised to wait 24 hours before returning to your normal activities.
Your throat may feel hoarse after the procedure. Your physician may recommend a throat lozenge or spray.
A chest x-ray may be performed 24 to 48 hours after the procedure to assess the removal of the contrast dye from the airways.
Notify your physician to report any of the following:
- fever and/or chills for longer than two to three days after the procedure
- redness, swelling, or bleeding or other drainage from the IV site
- extreme hoarseness or difficulty breathing
Your physician may give you additional or alternate instructions after the procedure, depending on your particular situation.
No comments:
Post a Comment