The blood contains several different types of cells, each with an important job in the body. All blood cells develop in the bone marrow, the spongy substance within our bones. The originator of all blood cells is an immature cell known as the stem cell. The stem cells give rise to committed or programmed stem cells, which then differentiate to form mature cells that circulate in our blood. There are 3 basic blood cell types:
- Red blood cells carry oxygen to, and carbon dioxide from, all bodily tissues in order to maintain effective organ function.
- Platelets, in combination with certain plasma proteins, help produce blood clots, which prevent bleeding.
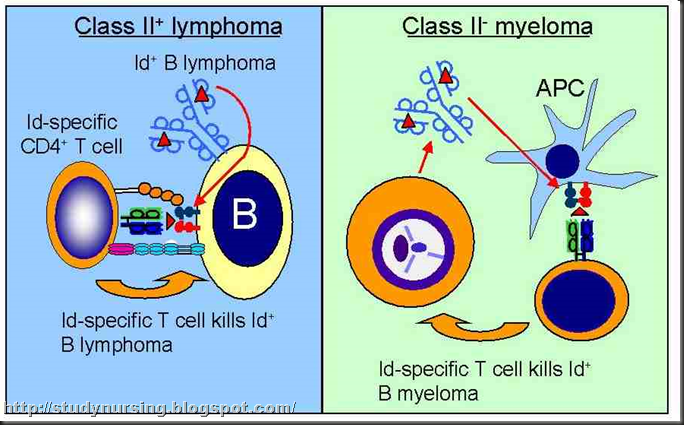
- White blood cells are part of the immune system, which protects the body from pathogens (things that can make us ill) such as infectious agents and precancerous cells. One of the most important subtypes of white blood cells is the lymphocyte. There are 2 major subtypes of lymphocytes: B lymphocytes and T lymphocytes (often called B cells and T cells). Some B lymphocytes mature into plasma cells. Plasma cells serve as producers of important protective proteins, called antibodies, which circulate and bind to various pathogens, rendering them harmless and susceptible to removal by other white cell components.
- Most plasma cells reside in the bone marrow, and myeloma, accordingly, usually occurs within the marrow-containing large bones of the body, such as the skull, vertebrae (spine), and hips.
- Because they are present throughout the bone marrow, plasma cells that have undergone malignant transformation do so in clumps and usually at many sites, which explains the terminology "multiple myeloma." When only one site is detectable, it is referred to as a solitary plasmacytoma, and these respond dramatically to local radiation or surgical excision. However, the recurrence rate is high, and they may recur years later as solitary or multiple tumors.
- Normal plasma cells produce antibodies, also called immunoglobulins (Ig). The abnormal plasma cells in myeloma do not produce the normal vast array of different immunoglobulins. Instead, myeloma cells may produce an abnormal immunoglobulin called a monoclonal protein, or M protein. (Monoclonal means that all proteins produced by this cell line have exactly the same identity and the same impaired function, which is essentially a deficiency.) Accordingly, most patients with myeloma have difficulty fighting off infections.
- Plasma cell tumors in the bone marrow crowd out the normal components of the marrow, resulting thereby in decreased numbers of red blood cells, platelets, and other white blood cells. This problem then results in fatigue and shortness of breath (decreased red cell count), bleeding or easy bruising (low platelet count), and increased susceptibility to infections (low white blood cell count).
- In myeloma, the abnormal plasma cells eventually invade and destroy the outer, hard layer of bone. The destruction of bones (osteolysis), typically occurring in small areas at different sites, may lead to serious problems. Even a small osteolytic lesion can cause the bone to fracture and collapse. The net effect may be problems with mobility, severe pain, and in the presence of spinal involvement, moderate-to-severe nerve damage.
- Boney destruction is often associated with high levels of blood calcium (hypercalcemia.)
- Production of M protein by the abnormal plasma cells causes high protein levels in the blood. The extra protein can lodge in the kidneys and obstruct blood flow. The abnormal protein can be directly toxic to the cells in the kidneys as well. The kidneys may become functionally impaired and ultimately fail altogether as a result of the protein blockage.
- In some cases of myeloma, excess protein in the blood can cause a condition called hyperviscosity syndrome. The type and amount of immunoglobulin protein can result in thickening the blood beyond normal blood viscosity, which may result in alteration in a variety of bodily, including mental, processes. This syndrome accounts for fewer than 5% of people with myeloma.
- Not everyone with myeloma has bone or kidney involvement at the time of diagnosis, but if the disease progresses without treatment, these problems may ultimately arise.
- Cryoglobulinemia: People with this rare condition produce a protein that precipitates, or falls out of solution, when the blood is exposed to cold temperatures.
- Amyloidosis: This rare complication occurs mostly in people whose myeloma produces the light chain components of immunoglobulins. The light chains combine with other substances in the blood to form a sticky protein called amyloid, which impairs the function of whichever organ in which it may accumulate.
- The most common monoclonal protein in myeloma is the IgG type. This means that the immunoglobulin is comprised of 2 IgG heavy chains and 2 light chains, either 2 kappa or 2 lambda. When the abnormal M protein is identified in myeloma, it is most often an IgG kappa type. However, any other combination is possible.
- Less common, but still prevalent, are IgA-producing myeloma cells.
- IgM myeloma is much less common.
- IgD and IgE myelomas are very rare.
- Some myelomas produce an incomplete immunoglobulin consisting of light chains only, known as Bence-Jones proteins, which are not identified by blood tests but readily identified in urine.
- Some rare diseases are associated with plasma cell overproduction of heavy chains only. These are referred to as heavy chain diseases. Heavy chain diseases may or may not be similar to myeloma in their characteristics.
- Nonsecretory myeloma occurs in about 1% of myelomas and represents malignant plasma cells that do not produce any immunoglobulin chains, heavy or light.
- People with MGUS produce small amounts of monoclonal protein, but they have none of the symptoms or complications of myeloma.
- MGUS is much more common than myeloma. The incidence of MGUS increases with age. It is uncommon in young individuals and reaches an incidence of approximately 3% in people aged 70 years and older.
Incidence
Myeloma is the second most common blood cancer, but it is not a common cancer. About 15,270 people were expected to be diagnosed with multiple myeloma in the United States in 2004, almost equally distributed between men and women. About 11,070 Americans were expected to die of multiple myeloma in 2004.
- Myeloma is predominantly a cancer of older people. More than 80% of people with myeloma are aged 60 years or older.
- Myeloma is nearly twice as common in African Americans as in Americans of European, Hispanic, or Asian descent.
Myeloma Causes
The cause of myeloma is unknown. Several factors have been linked to myeloma, including genetic abnormalities, exposures to certain chemicals and other conditions in the workplace (petrochemical industry workers, leather workers, book binders, cosmetologists, shipyard workers, metallurgic industry workers), exposure to very large doses of radiation, certain viral infections, and immune system dysfunction. However, how any of these factors actually causes myeloma is unknown. Some people who develop myeloma have none of these risk factors.
Myeloma Symptoms
The symptoms of myeloma depend upon the extent of plasma cell disease and the specific properties of the M proteins secreted.
- Unexpected early osteoporosis can be a sign of myeloma. A person considered too young to be "hunched over" or who notices progressive loss of height or alteration in spinal curvature may have myeloma in the vertebral bones.
- Osteolytic bone lesions: The most common symptom is pain. The most frequently affected areas of the skeleton are the ribs and the spine, resulting in chest wall or back pain. In more advanced myeloma, bone degeneration can cause bones to press on nerve structures, resulting in tingling, numbness, burning sensation, loss of function of a limb or joint, or even paralysis.
- Hypercalcemia and kidney damage: Common symptoms include fatigue, nausea, vomiting, loss of appetite, muscle weakness, constipation, decreased urine production, dehydration and increased thirst, restlessness, difficulty in thinking or concentrating, and confusion. Patients without hypercalcemia but with kidney damage may be have no symptoms or may complain of foamy urine.
- Hyperviscosity syndrome: Symptoms associated with sludging in the blood vessels may include spontaneous bruising or bleeding (from the mouth, nose, or internally), visual problems (due to bleeding and vascular problems in the eye [retinopathy]), neurologic problems (lethargy, confusion, sleepiness, headache, problems with sensation or movement in one area of the body [neuropathy], stroke), and shortness of breath or chest pain (due to congestive heart failure caused by an increased blood volume meant to dilute the blood).
- Low red blood cell count (anemia): Symptoms include fatigue, paleness, and mild shortness of breath.
- Low white blood cell count: Symptoms include increased frequency of and susceptibility to infections.
- Low platelet count: Symptoms include spontaneous bruising, bleeding, or tiny red spots on the skin caused by slowed or unproductive blood clotting. Bleeding can also be internal. Undetected bleeding may occur in the brain or digestive tract.
- Cryoglobulinemia: The usual symptoms are increased sensitivity to cold and/or pain and numbness in the fingers and toes during cold weather.
- Amyloidosis: The symptoms are related to malfunction or failure of organs or structures infiltrated by amyloid deposits. These symptoms include problems such as heart failure, liver failure, kidney failure, and blood vessel damage.
When to Seek Medical Care
Early in the disease, symptoms may be subtle. The symptoms of myeloma generally are nonspecific, meaning they may be caused by many different conditions unrelated to cancer. Any of the following warrant a visit to a health care provider:
- Unexplained and constant pain, especially in the spine, ribs, pelvis, head, arm, or leg
- Constant fatigue or weakness
- Frequent infections
- Unexplained weight loss
- Spontaneous bleeding or easy bruising
- Unexplained vision problems
- Shortness of breath
- Unexplained nausea or persistent vomiting
- Problems thinking or concentrating
- Foamy urine
- Unexpected spinal curvature or rapid loss of height
- Unexplained chronic numbness or tingling in the fingers or toes
Exams and Tests
In many cases, myeloma is discovered when blood tests, done as part of a routine physical examination or for some other reason, reveal anemia or a high level of protein. A urine test may show protein in the urine. It is important to do both a blood test and a urine test for proteins when testing for myeloma. Occasionally, a chest x-ray will identify significant osteoporosis in the vertebral (spine) bones, or even compression of a vertebral body. Such findings should prompt further testing to detect the underlying cause.
At some point in this testing process, the health care provider refers the person to a blood cancer specialist (hematologist-oncologist). Once the evaluation is completed and the presumptive diagnosis confirmed, the findings are usually presented to the patient in person and also to the patient's health care provider in writing.
Blood and urine tests
Complete blood cell count (CBC count): This test measures the hemoglobin (the amount of oxygen-carrying protein) as well as the numbers of different cells in the blood.
The most important measures in the CBC are as follows:
- Hemoglobin and hematocrit: Hemoglobin is the amount of oxygen-carrying protein in the blood. Hematocrit is the percentage of red blood cells in the blood. A low hemoglobin or hematocrit value indicates anemia.
- White blood cell count: This is usually abbreviated WBC count and is a measure of how many white blood cells there are in a certain volume of blood.
- Platelet count: Platelets are an important part of the clot that forms when a blood vessel is broken or torn. A low platelet count may indicate a tendency to bleed or bruise.
Blood chemistry panel: This set of tests gives a broad look at levels of various substances in the blood that may indicate the severity of myeloma and myeloma-related complications.
- Protein: Two types of protein are commonly measured in the blood: albumin and globulins. A high level of total protein in the blood may be a clue to the presence of myeloma; a high level of globulins is even more suggestive.
- Calcium: A high level of calcium suggests active reabsorption of bone and thus active myeloma.
- Lactate dehydrogenase (LDH): A high level of this enzyme may indicate active myeloma.
- Blood urea nitrogen (BUN) and creatinine: These are indicators of kidney function. Elevated levels, particularly of creatinine, represent kidney dysfunction.
Serum protein electrophoresis (SPEP): This test measures the levels of various proteins in the blood. It is the best test for detecting and measuring the abnormal monoclonal protein level associated with myeloma.
Urine protein electrophoresis (UEP): This test measures the levels of various proteins in the urine. In light-chain-only disease, the abnormal proteins are usually detectable only in urine, not in blood.
Immunofixation (or immunoelectrophoresis, IEP): This test can reveal the specific type of abnormal protein produced by the myeloma.
24-hour urine test for Bence-Jones or light chain proteins in the urine: This test measures the actual amount of myeloma protein being produced by the kidneys.
Serum free light chain measurement: This test measures the amount of light chain, a type of myeloma protein, in the blood.
Prognostic indicators: Various blood tests are used to predict the outcome (prognosis) for an individual. Some of these are simple tests done in every laboratory; others are done only in specialized labs or in research settings. Many of these are not yet used widely but may be in the future. Depending on the situation, these tests may or may not be performed.
- Beta2-microglobulin (â2M): A high level of this normal protein indicates extensive disease and a thus a poorer prognosis.
- C-reactive protein (CRP): A high level of this inflammatory marker may indicate a poor prognosis.
- Lactate dehydrogenase (LDH): A high level of this normal enzyme indicates extensive myeloma.
- In cases of IgM myeloma, a serum viscosity test may be performed.
Examination of the bone marrow is necessary to make the diagnosis of myeloma and to estimate the extent of the disease. A bone marrow biopsy is the procedure to collect a sample of bone marrow.
- Two types of bone marrow samples are taken: Liquid bone marrow (an aspirate) and solid bone marrow within bone core (a biopsy). The biopsy is usually performed on the hip bone.
- The bone marrow is examined under a microscope by a pathologist, a physician who specializes in diagnosing diseases by examining cells and tissues.
- If plasma cells comprise 10-30% of the cells in the bone marrow, this supports the diagnosis of myeloma, in combination with M protein and X-ray findings.
- Bone marrow biopsy may be an uncomfortable, but relatively quick, procedure, so most patients receive some from of premedication to make them more comfortable. It can usually be performed in a medical office.
- Occasionally more involved tests may be performed on the bone marrow. Not all tests listed are routinely performed by the pathologist, but they can be requested by the patient's physician. These may be helpful in assessing prognosis and expected behavior of the myeloma.
- Chromosome analysis: This test identifies chromosome abnormalities in the abnormal plasma cells. Certain chromosome abnormalities are linked to poorer prognosis. Certain chromosomal abnormalities also imply that some specific treatments might be less effective. This test is therefore an important treatment guide.
- Plasmablastic morphology: This test examines the abnormal plasma cells and determines their level of maturity. Fewer mature plasma cells indicate a poorer prognosis.
- Bone marrow microvessel density: A high degree of new blood vessel development in the bone marrow indicates active tumor growth and thus a poorer prognosis.
- Plasma cell labeling index: A high level of this indicator of active plasma cell growth may indicate a poorer prognosis.
The tests most often used for testing myeloma are x-rays films and magnetic resonance imaging (MRI) scans.
- X-ray films: X-ray films give a general overview of bone damage. A skeletal survey includes x-ray films from every part of the body. Osteolytic lesions look darkened, "punched out," or mottled against the white bone substance on X-ray films. X-ray films can also reveal bone fractures or collapse, as in the vertebrae of the spine.
- MRI: MRI uses differences in magnetic vibrations between different types of tissue to give a detailed picture of body structures. MRI is a good choice to show greater detail of a site where myeloma is suspected of causing damage to nerves, blood vessels, or other soft tissues.
These tests are used not only to diagnose myeloma but also to monitor the disease's progress over time and to measure response to treatment. Thus, the specialist regularly repeats all or most of these tests to keep track of how the disease is progressing. Tracking the levels of normal and abnormal proteins in the blood is particularly useful in this regard.
In most people, treating the plasma cell tumors stops damage to the bones and kidneys and reverses complications due to low blood cell counts, hypercalcemia, and hyperviscosity. Blood cell counts and hemoglobin, protein, calcium, and other indicators return to normal or near normal levels when the disease is under control.
Staging
Like most cancers, myeloma is classified into various groups based on the extent of disease, how fast it is progressing, the type and amount of abnormal protein produced, and the types of symptoms and complications. Staging is important because it helps the specialist determine the optimal timing of treatment, the best type of treatment, and the outlook for remission and survival for each individual with myeloma. The types of plasma cells disorders are as follows:
- Monoclonal gammopathy of undetermined significance, or MGUS: In this condition, a small amount of monoclonal protein is produced, but it does not fulfill criteria for the diagnosis of myeloma. There is no associated anemia, infections, bone disease, or lowering of normal immunoglobulin levels. It is unknown whether this disease will progress. Because MGUS involves no symptoms or complications, it does not require treatment. Instead, the person undergoes regular follow-up and testing so that any progression to malignant disease can be detected early and treated promptly. This type accounts for about 1% of people with plasma cell disorders.
- Smoldering multiple myeloma: This condition involves the findings of abnormal plasma cells that produce a monoclonal protein, but no symptoms or complications of myeloma are present. This condition accounts for about 5% of all cases of myeloma. The disease may remain stable without progressing to active myeloma for years. In some people, it never does. Because the disease is not active, it does not require treatment. Like MGUS, smoldering myeloma requires careful follow-up and testing so that any progression to active myeloma can be detected early and treated promptly.
- Indolent multiple myeloma: People with this type of myeloma have an elevated number of abnormal plasma cells in the bone marrow that may or may not produce monoclonal protein. They also have mild anemia or a few bone lesions, but they have no symptoms. The disease may remain stable for long periods. Treatment begins at the first sign of any disease progression.
- Symptomatic multiple myeloma: This is the full, active form of myeloma. The number of plasma cells in the bone marrow is generally more elevated, with production of monoclonal protein, except in the case of nonsecretory myeloma. Other specific diagnostic criteria must be met before making the diagnosis of myeloma, such as degree of anemia, depression of normal immunoglobulin levels, level of calcium, and presence of bone lesions.
In myeloma, staging has traditionally been based upon the following criteria: level of hemoglobin (RBC level), degree of M protein elevation, serum calcium levels, and the presence of bone lytic lesions. Early stage disease is deemed to be stage I, while extensive disease is deemed stage III. Intermediate findings suggest stage II disease. Recently, a newer International Staging System has proposed the use of serum beta-2 microglobulin and albumin levels to determine stages I-III, suggesting that such markers may more accurately define treatment decisions and, potentially, outcome.
Myeloma Treatment
Primary health care providers will usually refer people with myeloma to a hematologist or oncologist.
- Although medical treatments are fairly standardized, different doctors have different philosophies and practices in caring for their patients.
- A person may want to consult with more than one specialist before selecting the hematologist-oncologist.
- Family members, friends, and health care providers are good resources to get referrals. Many communities, medical societies, and cancer centers offer telephone or Internet referral services.
- The doctor will present each type of treatment, give the pros and cons, and make recommendations based on published treatment guidelines and the doctor's experience.
- Treatment for myeloma depends on the stage. Factors such as age, overall health, and recurrence of myeloma are included in the treatment decision-making process.
- The decision of which treatment to pursue is made between the person's hematologist-oncologist (with input from other members of the care team) and family members, but the decision ultimately rests with the patient.
- For optimal treatment results, a person should be certain to understand exactly what will be done and why, and what to expect from the treatments that have been decided upon.
- A treatment plan is individualized for a specific situation.
- The most widely used therapies are chemotherapy, corticosteroids, and/or radiation therapy.
- Newer medications that are active against myeloma may be offered, either as single therapy or together with chemotherapy.
- Supportive care is given to treat complications and symptoms. Some potential supportive care medications include growth factors for anemia and medications to treat bone disease.
- Some patients may be referred for additional treatment, such as stem cell transplantation.
There is no cure for myeloma. The goal of medical therapy is complete remission. This means that there is no detectable monoclonal protein and the number of plasma cells in the bone marrow is normal (less than 5%) after treatment. Remission is not the same as cure. In remission, small numbers of myeloma cells may remain in the body, but they are undetectable using currently available technology and cause no symptoms.
- The objectives in achieving complete remission are preventing myeloma-related damage to bones, kidneys, and other organs; prolonging life; relieving symptoms; and preserving a good quality of life for as long as possible.
- Most patients in remission will eventually experience recurrent disease.
- The duration of remission depends on the stage of myeloma and varies by disease characteristics. Remission may be quite variable, lasting for a few months, or for many decades. Remission that lasts a long time is called durable remission, which is the goal of therapy. The duration of remission is a good indicator of the aggressiveness of the myeloma. Remission can also be considered partial. A partial remission (also called partial response) means that the level of monoclonal protein decreases after treatment to less than half its level before treatment. A very good partial response means that the level of monoclonal protein decreases by at least 90% from its level before treatment.
- Minor response: The level of monoclonal protein decreases but is still greater than half the original level.
- Stable disease/plateau phase: The level of monoclonal protein stays the same.
- Progression: The level of monoclonal protein worsens with treatment. This includes recurrent or refractory myeloma.
- Refractory myeloma: The disease is resistant to the treatment.
- The first line of therapy given for myeloma is often referred to as "induction therapy" because it is designed to induce a remission.
- If this treatment does not induce a complete remission, the person will probably be given a different treatment regimen. This is sometimes called "second-line therapy," or occasionally, "salvage therapy."
- Once the disease is controlled, the person may be given yet more treatment to maintain control. This is called "maintenance therapy."
- Some patients may have sufficiently aggressive myeloma to be considered candidates for stem cell transplantation, which is an intensive, high-dose chemotherapy regimen, followed by infusion of normal donor matched cells (in the form of an allogeneic stem cell transfusion, or followed by the reinfusion of the patient's stem cells, in the form of an autologous transplant). This form of treatment is often referred to as "consolidation therapy."
Medical Treatment
Standard first-line (primary) therapy for myeloma involves corticosteroid therapy, with or without chemotherapy. Supportive care is frequently given in conjunction with treatment. However, current investigations may eventually change the approach to first-line treatment of myeloma to nonchemotherapeutic approaches. Sometimes radiation therapy is added for people with significant bone damage.
Chemotherapy
Chemotherapy is the use of powerful drugs to kill cancer cells. Chemotherapy is a systemic therapy, meaning that it circulates through the bloodstream and affects almost all parts of the body. Ideally, chemotherapy can find and kill cancer cells throughout the body.
Unfortunately, chemotherapy also affects healthy cells, which accounts for its well-known side effects.
- The side effects of chemotherapy depend partly on the drugs used and the doses.
- Some people, due to variability in drug metabolism, tolerate chemotherapy better than others.
- The most common general side effects of chemotherapy include fatigue, increased susceptibility to infections, nausea and vomiting, loss of appetite, hair loss, sores in the mouth and digestive tract, muscle aches, and easy bruising or bleeding. Specific drugs may confer other specific side effects.
- Medications and other treatments are available to help people tolerate these side effects, which can be severe and, rarely, life-threatening, especially in the elderly.
- It is important that a patient review the expected outcomes and potential side effects of therapy with their health care provider prior to embarking on their selected course of treatment.
Clinical Trials
New therapies and novel ways to administer known therapies are continually under investigation for the treatment of multiple myeloma. These novel therapies come about as a result of favorable performance in earlier, monitored, national multi-institutional studies. Usually, a clinical trial is offered to patients in order to extend and confirm the earlier results of such studies. In order to receive such new therapies, a patient would have to agree to treatment by enrolling in a clinical trial.Ideally, the treating hematologist/oncologist will belong to a clinical trial network that provides up-to-date therapy and instant analysis of ongoing data. Patient enrollment in any clinical trial involves agreeing to a particular treatment plan that is exquisitely detailed by the physician and other members of the treatment team. A written protocol is provided to the patient and includes a fully detailed/informed written consent document.
The protocol, and its associated consent form, details the medications, all known side effects, and alternatives to treatment should there be failures in therapy or patient refusal to participate. As noted, the patient is fully apprised of the potential benefits and risks associated with such treatment, and consent is obtained in the presence of the treating physician and very likely other members of the treatment team.
Alternatively, a hematologist-oncologist may refer a patient to another institution to receive investigational treatment or intensive treatment, which may be otherwise unavailable at the current institution, such as stem cell transplantation.
Radiation therapy
Radiation therapy uses high-energy rays to kill cancer cells. It is considered a local therapy, meaning that it should be used to target areas of the body involved by myeloma. A radiation oncologist plans and supervises therapy.
- In myeloma, radiation is used primarily to treat solitary plasma cell tumors, larger tumors, or to prevent a pathologic fracture in a myeloma-compromised bone.
- In people with extensive disease, radiation may be applied to a larger area to kill off multiple sites of myeloma.
- Radiation may be used to relieve pain and other symptoms related to a small area of particularly severe bone damage.
- Total body irradiation (TBI), which involves the entire body, is administered only for people undergoing stem-cell transplantation.
- Depending on how and where the radiation is administered, it may cause certain side effects such as fatigue, loss of appetite, nausea, diarrhea, and skin problems. Radiation of lymph node areas may result in suppression of the immune system to varying degrees. Irradiation of underlying bone and the marrow within the bone may result in suppression of the blood counts.
- The schedule for radiation treatments depends on the dose and the treatment goals. Radiation is often administered in short bursts over several days or weeks in order to minimize side effects without losing therapeutic efficiency.
Stem-cell transplantation is often used as consolidation therapy after a patient has achieved a complete remission (CR), or after a second CR is achieved in recurrent disease. It is also used in patients who are unable to achieve a remission with first line, or so called standard, therapy.
- Stem-cell transplantation is more effective than conventional chemotherapy in killing myeloma cells. However, it is a physically and emotionally demanding treatment, so not everyone with myeloma is a candidate for such an aggressive approach. Stem cell transplantation is most often used for younger patients or selected older patients with a good performance status. It has been associated with higher remission rates, as well as longer remission and survival than those of standard-dose chemotherapy.
- This procedure involves the use of very high doses of chemotherapy to kill the aggressive cancer cells.
- The chemotherapy dose is designed to destroy the marrow, in essence to keep the marrow from spontaneously recovering and producing abnormal cells once again.
- The individual is then given a transfusion of healthy bone marrow stem cells. The number of cells infused is calculated to be sufficient to induce marrow recovery with the bone marrow stem cell precursors. Conceptually, an allogenic (from a tissue-matched family donor) stem cell transplant would be preferable, in order to infuse tumor-free stem cells. However, because myeloma is a disease of the elderly, few patients may meet criteria for such an aggressive approach, and those who undergo standard allogeneic transplantation are at higher risk of complications and death.
- Should one's own stem cells be used, the reinfusion after high-dose therapy is referred to as autologous (one's own). Autologous re-infusion, or transplantation, of stem cells is a frequent treatment recommendation for patients with aggressive myelomas. It may be the only recourse if an allogeneic donor is unavailable, but it is more tolerable and associated with better survival than standard allogeneic transplantation. Nevertheless, the outcome is less likely to result in myeloma-free survival because of the uncertainty that the autologous marrow is completely disease free.
- Nonetheless, early autologous transplant, compared with continuation of chemotherapy and delayed transplant in several studies, was associated with a longer symptom-free interval.
- Allogeneic transplant may be recommended for long-term control of disease; however, such an approach is associated with higher morbidity and mortality rates compared to younger patients and those with other diagnoses. Recently, however, there have been a number of clinical trials evaluating the outcomes of patients who have received less intensive, "nonmyeloablative" transplants, sometimes referred to as "mini-transplants." A tissue-compatible family donor is still required for such a procedure, but it is associated with lower mortality rates compared with those of standard allogeneic transplant. The idea behind such an approach is to administer lower doses of chemotherapy to minimize organ damage, and to use allogeneic stem cells to exert an immune reaction against the myeloma, called "graft versus myeloma" effect.
Supportive care is very important in the management of all cancers, and myeloma is no exception. The following issues should be addressed in controlling the complications of the disease:
- Bone stabilization: A class of drugs, the bisphosphonates, is able to slow bone damage, reduce the risk of fractures, and reduce pain due to thinning of bone. They also regulate calcium levels in the blood and possibly affect the immune system in ways that may help fight the myeloma. These drugs are given intravenously, generally once every 3-4 weeks. Examples include pamidronate (Aredia) and zoledronic acid (Zometa). Other bisphosphonates are undergoing development or further evaluation.
- Pain control: Osteolytic lesions and the resulting fractures can cause considerable pain. Patients with myeloma often require pain-reducing medications or radiation to painful lesions.
- Orthopedic care: The fractures from osteolytic damage can cause severe pain and disability. A bone specialist (orthopedist) may provide relief from pain and improve functionality of the affected bones, if necessary. Neurosurgeons, orthopedists, or interventional radiologists may offer a procedure called vertebroplasty (injection of bone cement) to stabilize affected bones in the spine.
- Growth factors: These agents boost production of new blood cells from the bone marrow and aid in recovery from the effects of chemotherapy.
Medications
Numerous chemotherapy and biological drug combinations have been used for multiple myeloma. Which type and combination of therapy depends on many factors, including the type and stage of myeloma, the ability to tolerate chemotherapy side effects, and if any previous treatment was rendered or if further treatment is planned, such as stem-cell transplantation. Hematologists/oncologists often work together regionally to decide which combination of chemotherapy and biological drugs are currently working best for their patients. Because of this regional collaboration, the drug combinations often vary and are able to change rapidly when improved results occur.
Chemotherapy
- Combinations of different chemotherapy drugs seem to be more effective than single agents. Several drugs with different mechanisms of action, when given together at lower doses, will likely increase the effectiveness of treatment, while reducing the likelihood of intolerable side effects.
- Several different standard combinations are used as induction therapy in myeloma, but the most widely used is the combination of vincristine (Oncovin), doxorubicin (Adriamycin), and the corticosteroid, dexamethasone (Decadron). This combination of drugs is referred to as "VAD". Another widely used combination is oral melphalan (Alkeran) with the corticosteroid prednisone. Which combination a person is given depends on the treatment plan and the experiences of the specialist and the medical center where treatment is received. For example, if a stem-cell transplant is part of a treatment plan, melphalan may not be given, since it can lower stem cell production.
- Recently, a new drug that interferes with cancer cell proteins (proteasome inhibitor), called bortezomib (Velcade) has been approved for second-line therapy. Studies are underway to determine its effect in first-line treatment and in combination with chemotherapy (see New drug therapy).
- The combinations of drugs are usually given according to a set schedule that must be followed strictly.
- In some situations, chemotherapy can be given in the hematologist-oncologist's office. In other situations, the person may need to stay in the hospital.
- One cycle includes the period of actual treatment (usually several days) followed by a period of rest and recovery (usually a few weeks).
- Standard treatment typically includes a set number of cycles, such as 4 or 6. Spacing out the chemotherapy this way allows a higher cumulative dose to be given while improving the person's ability to tolerate the side effects.
- Certain drugs widely used against myeloma-namely, melphalan, prednisone, dexamethasone, and new time-release forms of doxorubicin-are in pill form.
- Most people who receive intravenous (IV) chemotherapy will have a semi-permanent device placed in a vein, usually in the chest or upper arm. This device allows a person's medical team quick and easy access to blood vessels, both for administering medications and for collecting blood samples. These devices come in several types, usually referred to as "catheter," "port," or "central line."
Other drugs that are standard treatments for myeloma are corticosteroids (prednisone or dexamethasone) and thalidomide (Thalomid).
Corticosteroids are powerful drugs that have many different actions, including anti-inflammatory and anti-immunity activity. They are active against myeloma and reduce production of protein M. Prednisone is usually given with melphalan. Dexamethasone can be given with chemotherapy agents or alone for people who cannot tolerate chemotherapy drugs. It is also given with thalidomide.
A nonchemotherapeutic agent, thalidomide, has been increasingly used in the first-line treatment of multiple myeloma. This is considered an immunomodulatory agent and is usually given with a corticosteroid, such as prednisone or dexamethasone (Decadron). Thalidomide's actions may include decreasing the ability of cancer spread throughout the blood (antiangiogenesis), interfering with adhesion molecules, or enhancing release of cytokines (cancer fighting substances within the body). This drug may be associated with sleepiness, constipation, venous blood clots, and numbness and tingling in the tips of the extremities. It is absolutely contraindicated in pregnancy, as it causes birth defects. The drug is dispensed through a program that ensures that physicians have educated patients about the importance of contraception when taking the drug. Usually, aspirin or low-dose blood thinners, such as warfarin (Coumadin) are given in conjunction with thalidomide and corticosteroids.
New drug therapy
A new analogue of thalidomide, CC-5013, or lenalidomide (Revimid), purportedly has fewer side effects of thalidomide and appears to be more potent than thalidomide in laboratory studies. It is also an immunomodulatory agent, which has undergone early clinical evaluation for recurrent myeloma and newly diagnosed myeloma with encouraging results. Further clinical evaluation is necessary and ongoing. It has been evaluated as part of combined therapy with corticosteroids or chemotherapy drugs. Currently, other immunomodulatory drugs for myeloma are also undergoing development.
Bortezomib (Velcade) is the first of a new class of medicines called proteasome inhibitors. Proteasome inhibitors may preferentially disrupt a cancer cell's growth. It is currently approved for refractory myeloma, which has previously been treated with two other regimens. However, promising results from early clinical trials suggest that it may be more effective when used for earlier disease. Currently, clinical trials are underway to assess results for first-line treatment, and also to evaluate combination therapy using the drug with corticosteroids, other chemotherapy drugs, and thalidomide. Other proteasome inhibitors have recently been developed and are now undergoing early clinical evaluation.
Next Steps
Follow-up
After primary therapy for myeloma is complete, all appropriate diagnostic tests, including bone marrow aspiration and biopsy, are repeated to determine how well the therapy worked.
- The results of these tests will determine whether a remission has occurred.
- If the patient is in remission, the oncologist will recommend a schedule of regular testing and follow-up visits to monitor the remission and identify early relapse.
- Maintaining constant vigil via follow-up exams and tests is no less important than the therapy itself.
Prevention
There is no known way to prevent myeloma. A standard recommendation is to avoid the risk factors for the disease, but little is known concerning the risk factors for myeloma.
Outlook
The outlook for myeloma has somewhat improved over the past few decades as treatment has improved. However, the overall 5-year survival rate is about 30%, and nearly 11,000 people in the United States die of myeloma per year.
Support Groups and Counseling
Living with myeloma presents many new challenges for an affected individual and his or her family and friends. There may be many worries about how myeloma will affect someone and his or her ability to "live a normal life," that is, to care for family and home, to hold a job, and to continue the friendships and activities one enjoys.
Many people may feel anxious and depressed. Some people feel angry and resentful; others feel helpless and defeated. For most people with myeloma, talking about their feelings and concerns can be helpful.
- Friends and family members can be very supportive. They may be hesitant to offer support for a variety of reasons. If the affected person wishes to talk about their concerns, it is important to let them know to do so.
- Some people don't want to "burden" their loved ones, or they prefer talking about their concerns with a more neutral professional. A social worker, counselor, or member of the clergy can be helpful if one wishes to discuss his or her feelings and concerns about having myeloma. The hematologist or oncologist should be able to recommend someone.
- Talking to other people who have myeloma profoundly helps many people with myeloma. Sharing concerns with others who have been through the same thing can be remarkably reassuring. Support groups of people with myeloma may be available through the medical center where one is receiving treatment. The American Cancer Society also has information about support groups all over the United States. Technorati Tags: cancer,amyloidosis,anemia,antibody,Bence-Jones protein,blood cancer,bone marrow,bone pain,cryoglobulinemia,hypercalcemia,hyperviscosity,immunoglobulin,kidney failure,light chains,lymphocytes,M protein,monoclonal gammopathy of undetermined significance,MGUS,monoclonal protein,multiple myeloma,osteolysis,plasma cell cancer,renal failure,renal insufficiency,solitary plasmacytoma,chemotherapy,radiation,radiation therapy,stem cell transplant,stem cell transplantation,total body irradiation,TBI,myeloma
No comments:
Post a Comment