Pleurisy (PLOOR-iss-ee) is caused by swelling and irritation of the membrane that surrounds the lungs. It is usually a symptom of another illness. It is also called Pleuritic Chest Pain.
Causes
Pleurisy can develop from many things, including bacterial or viral infections of the lungs (such as pneumonia), TB, lupus, chest injury or trauma, a blood clot in the lung, or cancer. Sometimes a cause cannot be found. Doctors call this ideopathic (id-e-o-PATH-ik) pleurisy. Even though the cause isn't known, the problem can still be treated.
Signs/Symptoms
The hallmark of pleurisy is severe chest pain that starts suddenly. The pain is often strong or stabbing when you take a deep breath. It usually subsides or disappears between breaths. It's usually felt on one side of the stomach area or lower chest. Deep breathing and coughing often make it worse. You may also have a fever, pain when moving, or fast, shallow breathing. Typically, you will be able to point to the exact location of the pain. In some people, the pain spreads to the neck, shoulder, or abdomen.
Care
While your doctor looks for the cause, you will get medicine to ease the pain. This will help you breathe more easily too.
Risks
Some cases of pleurisy clear up by themselves, but it's more likely that your lung problems will get worse. Possible problems include pneumonia or fluid build-up in the lining of the lungs. Some problems can cause damage to the lungs and affect your ability to breathe.
WHAT YOU SHOULD KNOW
- Always take your medicine as directed. If you feel it is not helping, call your doctor. Do not quit taking it on your own.
- If you are taking antibiotics, continue to take them until they are all gone--even if you feel well.
- If you are taking medicine that makes you drowsy, do not drive or use heavy equipment.
- Quit smoking. It harms the lungs. If you are having trouble quitting, ask your doctor for help.
- To ease the pain:
- When you cough, hold a pillow tightly against your chest.
- Lie on the side that hurts.
- You may need to loosely wrap a 6 inch elastic ace bandage around your chest. You should unwrap it several times a day.
- To help keep your lungs free of infection, take 2 or 3 deep breaths and then cough. Do this often during the day.
- If you are coughing up sputum and milk seems to make the sputum thicker, do not eat or drink foods that contain milk.
- If you do not have to limit the amount of liquids you drink, drink 8 to 10 (soda-can size) glasses of water each day. This helps thin the sputum so it can be coughed up more easily.
- Use a humidifier to help keep the air moist and your sputum thin. This makes it easier to cough up the sputum. You must keep the humidifier free of fungus. Clean it every day.
- Rest until you feel better. You may return to work or school when your temperature is around 98.6 degrees F (37 degrees C).
Call Your Doctor If...
- You have a high temperature.
- You cough up yellow, green, gray, or bloody sputum.
- Your pain gets worse.
Seek Care Immediately If...
- You have blue or pale lips, fingernails, or toenails.
- You have increased trouble breathing even if the pain is less.
IF YOU'RE HEADING FOR THE HOSPITAL...
What to Expect While You're There
You may encounter the following procedures and equipment during your stay.
- Activity: At first you will need to rest in bed, with a few pillows to keep you sitting up a little. This will help your breathing. Do not lie flat. Once you are breathing more easily, you will be allowed to increase your exercise.
- Taking Vital Signs: These include your temperature, blood pressure, pulse (counting your heartbeats), and respirations (counting your breaths). A stethoscope is used to listen to your heart and lungs. Your blood pressure is taken by wrapping a cuff around your arm.
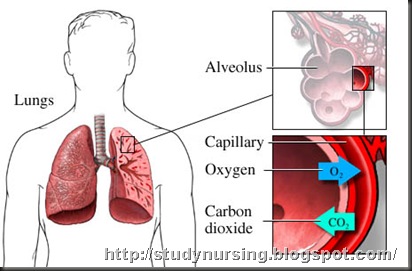
- Oxygen: Your body may need extra oxygen at this time. It is given either by a mask or nasal prongs. Tell your doctor if the oxygen is drying out your nose or if the nasal prongs bother you.
- Pulse Oximeter: While you are getting oxygen, you may be hooked up to a pulse oximeter (ox-IM-uh-ter). It is placed on your ear, finger, or toe and is connected to a machine. It tells how much oxygen is in your blood.
- ECG: Also called a heart monitor, an electrocardiograph (e-lec-tro-CAR-dee-o-graf), or EKG. The patches on your chest are hooked up to a TV-type screen or a small portable box (telemetry unit). This screen shows a tracing of each heartbeat. Your heart will be watched for signs of injury or damage that could be related to your illness.
- 12 Lead ECG: This test makes tracings from different parts of your heart. It can help your doctor decide whether there is a heart problem.
- Chest X-ray: This picture of your lungs and heart shows how they are handling the illness.
- Blood: Usually taken from a vein in your hand or from the bend in your elbow. Tests will be done on the blood.
- IV: A tube placed in your vein for giving medicine or liquids. It will be capped or have tubing connected to it.
- Medicines: You will be given medicine to ease the pain. This will help you breathe more easily also. You may also need antibiotics to fight infection.
- Coughing and Deep Breathing: It is important to do this often because it helps prevent infections in your lungs.
- To ease your pain during breathing, you may need to loosely wrap your rib cage with a 6 inch elastic bandage.
- Holding a pillow tightly against your chest when you cough can help reduce the pain. Lying on the side that is hurting, may also help ease the pain.
- Cold/Heat: A cool towel or heating pad (set on low) placed on the area that hurts may help ease the pain.
- Sputum Sample: If you are coughing up sputum, your doctor may need to send a sample to the lab. This sample may show what is causing your illness. It will also help the doctor choose the medicine you need.
- Other Care:
- Nerve Block: You may need this if your pain gets worse. This is a shot of pain-killers in the nerves serving the chest (intercostal) muscles.
Nursing Management
acute Pain may be related to inflammation/irritation of the parietal pleura, possibly evidenced by verbal reports, guarding/distraction behaviors, self-focus, and autonomic responses (changes in vital signs).
ineffective Breathing Pattern may be related to pain on inspiration, possibly evidenced by decreased respiratory depth, tachypnea, and dyspnea.
risk for Infection [pneumonia]: risk factors may include stasis of pulmonary secretions, decreased lung expansion, and ineffective cough.*
No comments:
Post a Comment