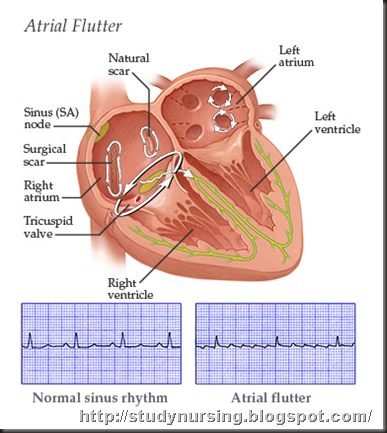
Atrial flutter is an abnormality of the heart rhythm, resulting in a rapid and sometimes irregular heartbeat. Such abnormalities, whether in the rate or regularity of the heartbeat, are known as arrhythmias.
The beating of the heart is controlled by electrical impulses.
- Under normal circumstances, these impulses are generated by the heart's natural pacemaker, the sinoatrial (SA) or sinus node, which is located in the right atrium.
- The impulse travels across the atria, generating a contraction of the atria.
- The impulse pauses very briefly at the atrioventricular (AV) node, which is located in the upper part of the muscular wall between the two ventricles. This delay gives the blood time to move from the atria to the ventricles.
- The impulse then moves down and through the ventricles, generating the ventricular contraction, which pumps the blood out of the ventricles.
Atrial flutter occurs when these electrical impulses take an abnormal path through the atria, typically circulating around the tricuspid valve in the right atrium.
- The abnormal path of the impulses makes the atria contract very rapidly, typically about 250-350 beats per minute. The normal heart rate is 50-100 beats per minute.
- These rapid contractions are slowed when they reach the AV node often with every second or third contraction reaching the ventricle.
- The heart beats in a regular rhythm, but it beats rapidly.
- This type of rhythm is called tachycardia (rapid heartbeat). Because atrial flutter comes from the atria, it is sometimes called a supraventricular (above the ventricles) tachycardia.
The main danger of atrial flutter is that the heart does not pump blood well when it is beating too fast. When blood is not pumped well, vital organs, such as the heart and brain, may not get enough oxygen from the blood.
Atrial flutter can come and go; it is then known as paroxysmal atrial flutter. More often, atrial flutter lasts for days to weeks and is known as persistent atrial flutter.
With proper treatment, atrial flutter is rarely life- threatening. Complications of atrial flutter, in particular stroke, can be devastating, but they can be prevented with medications ("blood thinners") such as warfarin
Causes
Atrial flutter may be caused by abnormalities of the heart, by diseases of the heart, or by diseases elsewhere in the body that affect the heart. Atrial flutter may also be caused by consuming substances that change the way electrical impulses are transmitted through the heart. Atrial flutter can occur after open heart surgery. In a few people, no underlying cause is ever found.
Heart diseases or abnormalities that can cause atrial flutter include the following:
- Decreased blood flow to the heart (ischemia) due to coronary heart disease, hardening of the arteries (atherosclerosis), and/or a heart attack
- High blood pressure (hypertension)
- Disease of the heart muscle (cardiomyopathy), especially associated with congestive heart failure
- Abnormalities of the heart valves, especially the mitral valve
- An abnormally enlarged chamber of the heart (hypertrophy)
Diseases elsewhere in the body that affect the heart include the following:
- Overactive thyroid gland (hyperthyroidism)
- A blood clot in a blood vessel in the lungs (pulmonary embolism)
- Chronic (ongoing, long-term) lung diseases, such as chronic obstructive pulmonary disease (COPD) and emphysema, that lower the amount of oxygen in the blood
Substances that may contribute to atrial flutter include the following:
- Alcohol (wine, beer, or hard liquor)
- Stimulants such as cocaine, amphetamines, diet pills, cold medicines, and even caffeine
Atrial flutter is closely related to another arrhythmia called atrial fibrillation. Atrial flutter and atrial fibrillation sometimes occur together.
Symptoms
Some people have no symptoms with atrial flutter. Others describe the following symptoms:
- Palpitations (a rapid heartbeat or a pounding sensation in the chest)
- A fluttering feeling in the chest
- Shortness of breath
- Anxiety
People with underlying heart or lung disease who experience atrial flutter may have these symptoms as well as the following more significant symptoms:
- Angina pectoris (chest or heart pains)
- Feeling faint or light headed
- Fainting (syncope)
When to Seek Medical Care
If a person experiences any of the symptoms suggestive of atrial flutter, a health care provider should be called for an appointment. If symptoms are severe or alarming, urgent medical attention should be sought.
If a person is taking any medication for atrial flutter and experiences a change or worsening of the symptoms, a health care provider should be called.
If a person has been diagnosed with atrial flutter and is being treated, medical attention should be sought immediately at a hospital emergency department if any of the following symptoms are experienced:
- Chest pain
- Feeling faint or light-headed
- Fainting
Diagnosis
Upon hearing about the symptoms, the health care provider (whether a primary care provider or a provider in the emergency department) may suspect an arrhythmia. Because many different arrhythmias can cause similar symptoms, the evaluation at first focuses on ruling out the most dangerous ones. One simple test, the electrocardiogram (ECG), can help tell a lot about what is happening with the heart.
The ECG measures and records the electrical impulses that control the beating of the heart.
- The ECG findings highlight irregularities in the heartbeat and abnormalities in the heart.
- In arrhythmias, the ECG tracings can help pinpoint the type of arrhythmia and where it comes from in the heart.
- The ECG also shows signs of heart attack, heart ischemia, abnormal heart enlargement (hypertrophy), conduction abnormalities, and certain chemical and electrolyte abnormalities in the heart tissue.
People sometimes have symptoms suggesting arrhythmias, but when the ECG is recorded, the result is normal. This may mean that the arrhythmia comes and goes (paroxysmal atrial flutter), a common condition, or it may mean an arrhythmia does not exist, and the heart feels odd or jumpy because of other factors, such as anxiety. If the ECG result is normal, an ambulatory ECG may be performed for 24 hours using a Holter monitor or for a longer period using an event monitor.
An ambulatory ECG involves a person wearing a monitoring device for a few days while going about normal activities. The purpose of an ambulatory ECG is to obtain documented proof of the arrhythmia. Proof is important because treatment depends upon identification of the arrhythmia.
- One device is known as a Holter monitor and usually records the heart rhythm on a continual basis for 24-48 hours.
- Some health care providers prefer that the device is worn for longer than 24-48 hours, with intermittent recording of the heart rhythm. In these cases, an event recorder is used.
- Both the Holter monitor and the event recorder work well. The important thing is to obtain ECG documentation of the arrhythmia, if it exists.
An echocardiogram is an ultrasound test that uses sound waves to make a picture of the inside of the heart while it is beating. In this test, an ultrasound probe is positioned on the outer chest wall, and the images obtained are viewed on a monitor.
- This test is performed to identify heart valve problems, to check ventricular function, or to look for blood clots in the atria.
- This safe, non-invasive test uses the same technique that is used to evaluate a fetus during pregnancy.
- This test is not always performed in the emergency department.
Occasionally, atrial flutter is detected in people with no symptoms when they see their health care provider for another reason. The health care provider may notice unusual heart sounds or an unusual pulse on physical exam, and he or she may order an ECG.
Self-Care at Home
Most people known to have atrial flutter take prescribed medications. Any stimulants that have previously provoked the atrial flutter should be avoided, and a health care provider should be consulted before any new medications, herbs, or supplements are taken.
Medical Treatment
Most people with atrial flutter have some form of underlying heart disease. They require medical treatment to reduce their heart rate and to maintain a normal sinus rhythm (normal heart rhythm). The goals of treatment are to control the heart rate, to restore a normal heart rate and sinus rhythm, to prevent future episodes, and to prevent stroke.
Control heart rate: The first treatment goal is to control the ventricular rate.
- If a person experiences serious clinical symptoms, such as chest pain or congestive heart failure related to the ventricular rate, the health care provider in the emergency department will decrease the heart rate rapidly with IV medications or controlled electrical shock (defibrillation) performed under anesthesia. Defibrillation is a technique that uses electrical current to shock the heart back to a normal sinus rhythm. Defibrillation is sometimes called DC cardioversion.
- Defibrillation is performed by connecting a device called an external defibrillator to the chest with patches or paddles.
- When this technique is performed in a hospital, an anesthetic drug is first given so the person is fully sedated and asleep during the procedure; no pain is associated with the procedure.
- Defibrillation works very well; more than 90% of people convert to a normal sinus rhythm. For many, however, this is not a permanent solution-the arrhythmia often returns.
- Defibrillation itself increases the risk of stroke and thus, if time allows, requires pretreatment with an anticoagulant medication, usually for three weeks.
- If no serious symptoms have occurred, the person may be given medications by mouth.
- Sometimes, a combination of oral medications is required to control the heart rate.
- In some people, an invasive procedure called radiofrequency catheter ablation may provide long-term successful treatment, and no additional medications may be needed. Radiofrequency catheter ablation is a technique that electronically burns and destroys some abnormal conduction pathways in the atria.
- The abnormal pathways are located, and a catheter is placed at this precise location in the conduction system.
- After proper placement, the catheter delivers radiofrequency energy that interrupts (ablates) a portion of the abnormal electrical conduction pathway. This ablation inactivates the abnormal pathway to provide the normal flow of electrical impulses.
- This technique is safe. When it works, atrial flutter may be permanently cured. Radiofrequency catheter ablation has few complications and, unlike surgery, requires little recovery time.
Restore and maintain a normal rhythm: Some people with newly diagnosed atrial flutter convert to a normal rhythm spontaneously in 24-48 hours; however, the atrial flutter may recur. The goal of treatment is to keep the heart rate normal and to prevent the heart from beating too fast.
- Not everyone with atrial flutter needs anti-arrhythmia medication.
- The frequency with which the arrhythmia returns and the symptoms it causes partly determine whether anti-arrhythmia medication is indicated.
- Medical professionals carefully tailor each person's anti-arrhythmia medication to produce the desired clinical effect without making the dose too high.
- Most of these anti-arrhythmia medications cause unwanted side effects, which limit their use.
Prevent future episodes: Prevention usually involves taking daily medication to keep the heart in a normal rhythm.
Prevent stroke: Stroke is a devastating complication of atrial flutter. Stroke occurs when a piece of a blood clot formed in the heart's left atrium breaks off and travels to the brain, where it blocks blood flow.
- Coexisting medical conditions, such as coronary heart disease with atrial flutter, significantly increase the risk of stroke.
- Most people with atrial flutter, including all people older than 65 years, should take a blood-thinning drug called warfarin (Coumadin) to lower this risk. Warfarin blocks the action of certain factors in the blood that promote clotting. In the short term, most patients are put on IV or subcutaneous (administered by injection under the skin) heparin, a drug that immediately decreases the risk of blood clots. A decision is then made whether oral warfarin is needed on a long-term basis.
- People at a lower risk of stroke and those who cannot take warfarin may use aspirin. Aspirin is not without its own side effects, including bleeding problems and stomach ulcers.
Medications
The choice of medication depends on the underlying cause, other medical conditions and overall health, and other medications being taken. Ironically, many anti-arrhythmia medications may induce abnormal heart rhythms.
Anti-arrhythmia medications
- Miscellaneous anti-arrhythmia medications: They reduce the frequency and duration of atrial flutter episodes and thus can prevent future episodes. They are often given to prevent the return of atrial flutter after defibrillation. The most commonly used drugs are amiodarone (Cordarone, Pacerone), sotalol (Betapace), propafenone (Rythmol), and flecainide (Tambocor).
- Digoxin (Lanoxin): This medication decreases the conductivity of the electrical impulses through the SA and AV nodes, slowing down the heart rate. Digoxin is not used as much as it was before beta-blockers and calcium blockers became available, except if the person has underlying heart failure due to a poorly functioning left ventricle.
- Beta-blockers: These drugs decrease the heart rate by slowing conduction through the AV node, decreasing the heart's demand for oxygen, and by stabilizing the blood pressure. Examples include propranolol (Inderal) or metoprolol (Lopressor Toprol XL).
- Calcium channel blockers: These drugs also slow down the heart rate by slowing AV node conduction. Verapamil (Calan, Isoptin) and diltiazem (Cardizem) are examples of calcium channel blockers.
- Dofetilide (Tikosyn): Administration of this oral anti-arrhythmic drug must be initiated in the hospital over a three day period. Hospitalization is needed to closely monitor the heart rhythm during the initial dosing period. If the atrial fibrillation responds favorably during the initial dosing, a maintenance dose is established to be continued at home.
Other drugs
- Anticoagulants: These drugs reduce the ability of the blood to clot, thus reducing the risk of an unwanted blood clot forming in the heart or in a blood vessel. Atrial flutter increases the risk of such blood clots forming in the left atrium. Warfarin (Coumadin) is the most common drug used for clot prevention caused by arrhythmias.
Prevention
Although atrial flutter cannot always be prevented, leading a healthy lifestyle may reduce the chance of experiencing coronary heart disease that can lead to atrial flutter.
The best way to prevent coronary heart disease is to practice "heart healthy living" as recommended by the American Heart Association.
- Do not smoke.
- Engage in moderately strenuous physical activity for at least 30 minutes a day.
- Eat nutritious foods that are low in cholesterol and other fats.
- Maintain a healthy weight.
- Control high blood pressure (hypertension) and high cholesterol.
If a person has already experienced an episode of atrial flutter, a health care provider should be seen regularly and his or her treatment recommendations should be strictly followed.

No comments:
Post a Comment