Cardiac catheterization is a test to check your heart and coronary arteries. It is used to check blood flow in the coronary arteries, blood flow and blood pressure in the chambers of the heart, find out how well the heart valves work, and check for defects in the way the wall of the heart moves. In children, this test is used to check for heart problems that have been present since birth (congenital heart defect).
The purpose of cardiac catheterization is to find out if you have disease in your coronary arteries (atherosclerosis). If you have atherosclerosis, this test can pinpoint the size and location of fat and calcium deposits (plaque) that are narrowing your coronary arteries. Results from cardiac catheterization help determine whether treatment with bypass surgery or percutaneous coronary intervention (PCI), such as angioplasty, may be effective.
Percutaneous coronary intervention (PCI) is similar to cardiac catheterization but it is used to open up a narrowed coronary artery. With PCI, your doctor guides a thin flexible tube (catheter) into the narrowed coronary arteries to open them using special tools and to improve blood flow to your heart. The two common types of PCI are:
- Angioplasty with stenting. The angioplasty is done by attaching a small balloon to the catheter. Once the catheter has been guided to the proper location in a coronary artery, the balloon is inflated. The pressure from the inflated balloon presses the plaque against the wall of the artery to improve blood flow. Once the plaque is compressed using angioplasty, a small expandable wire tube called a stent is inserted into the artery to hold it open. Reclosure of the artery is less likely to occur after angioplasty followed by stenting than after angioplasty alone. This is the most common procedure performed. See a picture of angioplasty.
- Atherectomy. This may be done during cardiac catheterization to open a partially blocked coronary artery. Once the catheter reaches the narrowed portion of the artery, a cutting device, a whirling blade (such as a rotoblade), or a laser beam is used to remove the plaque. This procedure is done in combination with balloon angioplasty or stenting.
Other tests can be done during cardiac catheterization to find heart problems. An X-ray test called a ventriculogram measures how well blood flows through the left side of your heart. The test looks at the movements of the wall of the left ventricle and the heart valves.
Why It Is Done
Cardiac catheterization and coronary artery disease
Cardiac catheterization is done to:
- Check blood flow and blood pressure in the chambers of the heart.
- Check blood flow in the coronary arteries and, if you have coronary artery disease (CAD), determine whether surgery or another type of procedure, such as angioplasty with stenting, is needed to open the blocked blood vessels.
Other reasons for having a cardiac catheterization
Cardiac catheterization is also done to:
- Check the pumping action of the heart.
- Find out if a congenital heart defect is present and how severe it is. Cardiac catheterization sometimes can also be used to help correct the defect.
- Check blood flow through the heart after surgery.
- Find out how well the heart valves work.
How To Prepare
Tell your doctor if you:
- Are allergic to the iodine dye used in the contrast material or any other substance that contains iodine.
- Have asthma or have ever had a serious allergic reaction (anaphylaxis) from any substance, such as the venom from a bee sting.
- Are allergic to any medicines and whether you are taking any erection-enhancing medicines, such as sildenafil (Viagra), tadalafil (Cialis), or vardenafil (Levitra). This test may require the use of nitrate medicine, such as nitroglycerin, that can cause severely low blood pressure if you have taken an erection-enhancing medicine within the previous 48 hours.
- Have any bleeding problems or take blood-thinning medicine (anticoagulant).
- Are or might be pregnant.
- Have kidney disease. The contrast material used during cardiac catheterization can cause kidney damage in people who have poor kidney function. If you have a history of kidney problems, blood tests (creatinine, blood urea nitrogen) may be done before the test to confirm that your kidneys are functioning properly.
- Have diabetes, especially if you take metformin (Glucophage). Your doctor may instruct you to stop the medicine 48 hours before the test.
Arrange for someone to take you home after the test. You may not have to stay in the hospital overnight.
Do not eat or drink (except for a small amount of water) for 6 to 12 hours before the test. If you are taking any medicines, ask your doctor whether you should take them on the day of the test.
Before the test, remove any necklaces, bracelets, rings, or other jewelry. You should also remove nail polish from your fingernails and toenails.
Be sure to empty your bladder completely just before the test.
How It Is Done
This test is performed in the cardiac catheterization laboratory ("cath lab") by a cardiologist. See a picture of a cardiac catheterization lab.
You will be asked to lie on a flat table under a large X-ray machine. Several small metal leads (electrodes) will be attached to your legs and arms with a special paste or gel. These leads are connected to an electrocardiogram (EKG, ECG) machine that continuously records the electrical activity of your heart during the test.
A device called a pulse oximeter that measures oxygen levels in your blood and monitors your pulse may be clipped to your finger.
An intravenous (IV) needle will be inserted into a vein in one of your arms to give you fluids or medicine during the procedure. You will receive a medicine to help you relax (sedative) through the IV line. You may be awake during the procedure. But even if you are awake, the sedative may make you so sleepy that you may not remember much about the procedure.
The thin flexible tube (cardiac catheter) is usually inserted in your groin (femoral artery). Other sites that may be used are the crease of your elbow (brachial artery) or your wrist (radial artery). The catheter insertion area will be shaved and cleansed with an antiseptic solution before the test. Sterile towels will be draped over your arm or leg, except for the area over the catheter insertion site.
A local anesthetic will be injected into the skin at the insertion site. A blood vessel is punctured by a special needle or exposed by making a small incision in the skin so that the catheter can be passed into the blood vessel. The catheter is slowly advanced through the blood vessel into your body. The catheter tip is moved into various positions in the heart's vessels and chambers while the doctor watches its progress on the imaging screen. Pressures within the heart chambers can be measured. Blood and heart tissue samples may also be removed through the catheter, if necessary.
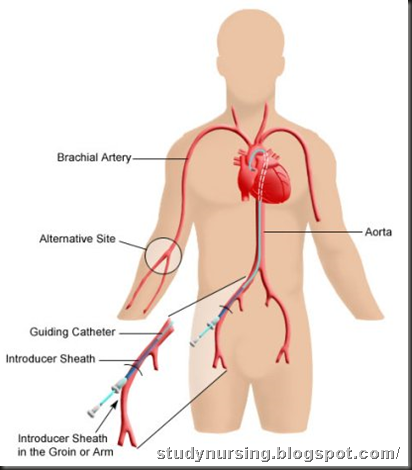 placement of a cardiac catheter(Click here to see detailed picture).
placement of a cardiac catheter(Click here to see detailed picture).
You may be asked to hold your breath or move your head slightly to provide clear views of the heart and its blood vessels.
A small amount of dye (contrast material) will be injected through the catheter into your heart chamber or one of your coronary arteries. Pictures show the arteries as the dye moves through them. You may be asked to cough to help clear the contrast material out of your heart or breathe deeply and hold your breath.
It is important to lie as still as possible, since motion can make the images blurry or hard to interpret. A health professional will help you stay comfortable and will help you resist the urge to move around. Be careful not to touch the sheets or reach for your groin area because you may contaminate the sterile areas and increase the risk of infection.
Your doctor may allow you to watch the video monitor so you can see the images of your heart and coronary arteries.
You may be given nitroglycerin to help open up your coronary arteries. Or you may be given an injection of a medicine (ergonovine maleate) that causes the coronary arteries to narrow. You may be asked to breathe into a special mouthpiece to help measure the flow of oxygen in your circulating blood.
After the test
The catheter will be removed from the insertion site. To prevent bleeding, the site may need to be closed using pressure, stitches, or a special seal. For example, if the catheter was inserted in your wrist or groin, firm pressure will be applied to the area for about 10 minutes to stop the bleeding. Then a pressure dressing will be placed over the area. If the catheter was inserted in your elbow, a few stitches will be used to close the wound.
The entire procedure usually takes about one hour, but it may take longer if additional tests are required. The length of the test is not an indication of the seriousness of your condition. After the test, you will be taken to an observation room and a health professional will periodically monitor your heart rate, blood pressure, and temperature and check for signs of bleeding at the insertion site. The pulse, color, and temperature of the arm or leg in which the catheter was inserted will also be checked periodically.
If the catheter was inserted in your leg, you may have to lie in bed with your leg extended for several hours (such as 4 to 12 hours), depending on the exact procedure used and your medical condition. After that, you can move about freely, but you should avoid strenuous activity for at least 1 to 2 days. A child who has had cardiac catheterization may need to be held by a parent for several hours after the test to prevent the child from moving his or her leg.
You should drink plenty of liquids for several hours after the test. This will prevent dehydration and help flush the contrast material out of your body.
Depending on the results of the test, you may be sent home either after a short observation period (such as 6 hours) or on the next day. If any stitches were placed in your arm, they may be removed in 5 to 7 days.
How It Feels
You will feel a sharp sting when the local anesthetic is injected to numb your skin over the catheter insertion site. When the catheter is inserted, you may feel a brief, sharp pain. The movement of the catheter through your blood vessel may cause a feeling of pressure, but it is not usually considered painful. People commonly experience skipped heartbeats for a few seconds when the catheter touches the walls of the heart.
If a dye (contrast material) is injected, you may feel warm and flushed and have a metallic taste in your mouth. Some people feel sick to their stomach or have a headache. You also may feel nauseous or lightheaded, have chest pain, irregular heartbeats, an urge to cough, mild itching, or hives from the contrast material. If you have any of these symptoms, tell your doctor how you are feeling.
The temperature in the catheterization lab is kept cool so that the equipment does not overheat. For many people, the most difficult aspect of the test is having to lie still for an hour or more on the hard table. You may feel some stiffness or cramping.
Call your doctor immediately if you have chest pain, extreme shortness of breath, dizziness, trouble speaking or swallowing, or paralysis in any part of your body during or after the test.
You may experience some soreness and bruising at the insertion site. This is temporary and should disappear within 2 weeks. It is normal for the site to feel tender for about a week. Call your doctor immediately if:
- Your arm or leg becomes pale, cold, painful, or numb.
- Redness, swelling, or discharge from the catheter insertion site develops.
- You have a fever.
Risks
Complications of cardiac catheterization are rare, but they can be life-threatening. Serious complications are more likely to occur in people who are critically ill or elderly. Serious complications may include:
- Heart attack or stroke. On rare occasions, the catheter tip can dislodge a blood clot or some debris from the inside wall of the artery. The clot or debris can travel through the bloodstream until it lodges in a smaller artery, blocking the blood flow.
- Blockage of blood flow to the arm or leg below the area where the catheter was inserted. Surgery may be needed to restore the blood circulation.
- Irregular heartbeats (arrhythmias). In rare cases, this procedure may produce a persistent abnormal heart rhythm. The abnormal rhythm usually corrects itself or becomes normal after treatment with medicine. In some cases, an electrical shock (electrical cardioversion) may be needed to restore a normal rhythm.
- Kidney damage. In rare cases, the contrast material can damage the kidneys, possibly causing kidney failure. People with diabetes and kidney disease are at greatest risk for kidney damage.
- Infection and inflammation of the membrane that lines the heart (endocarditis).
- An abnormal collection of fluid in the space between the heart and the sac that surrounds it (cardiac tamponade).
- A buildup of air in the space between the lung and the chest wall (pneumothorax).
- Puncture of the heart or one of its blood vessels. This may require draining of the catheter or immediate open-heart surgery to repair.
- Liver tears, which are more likely in babies and children than in adults.
- Allergic reaction to the contrast material, with hives and itching and, rarely, shortness of breath, fever, and shock. These allergic reactions can usually be controlled with medicines.
Less serious complications include:
- Pain, swelling, and tenderness at the catheter insertion site.
- Irritation of the vein by the catheter (superficial thrombophlebitis). This can usually be treated with warm compresses.
- Bleeding at the catheter site.
- A bruise where the catheter was inserted. This usually goes away in a few days.
- Difficulty urinating after the procedure.
There is always a slight risk of damage to cells or tissues from being exposed to any radiation, including the low levels of X-ray used for this test. However, the risk of damage from the X-rays is usually very low compared with the potential benefits of the test.
Results
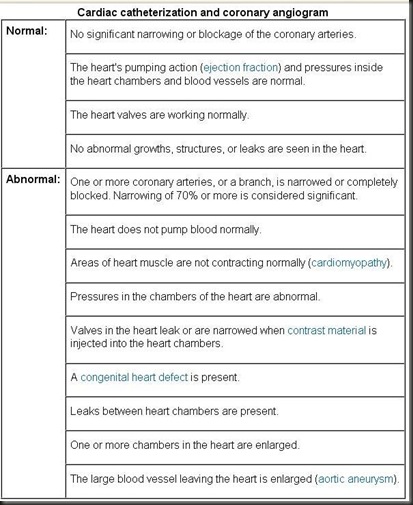
Cardiac catheterization is a test to check your heart and coronary arteries.
Test results will be reviewed by a cardiologist and will be available after the procedure. Your doctor will be able to talk to you about some of the results immediately after the test.
What Affects the Test
Reasons you may not be able to have the test or why the results may not be helpful include:
- Extreme anxiety that causes high blood pressure and irregular heartbeats.
- Kidney or liver failure.
- Inability to follow directions during the procedure.
What To Think About
- About 1 in 5 people who have angiography is found to have normal coronary arteries.
- This test usually is not done on people who have had severe allergic reactions to contrast material, poorly controlled heart failure, life-threatening heart rhythm problems, or advanced kidney disease.
- Cardiac catheterization is not usually done during pregnancy because the radiation could damage the developing fetus. But in a life-threatening emergency, this procedure may be necessary to help save a pregnant woman's life. In such cases, the fetus is protected as much as possible from radiation exposure with a lead apron.
- If you are breast-feeding, use formula for 1 to 2 days after the test.
- In the future, electron-beam CT (EBCT) or MRI of the coronary arteries may be used instead of an angiogram to evaluate symptoms of coronary artery disease.
No comments:
Post a Comment