Almost everyone who has a critically ill friend or relative may expect to hear the term, respiratory failure. Although failure to breathe normally was recognized even in ancient times as an ominous sign, the term, "respiratory failure," did not appear in the medical literature until the 1960s. Doctors now understand that respiratory failure is a serious disorder caused by a variety of different medical problems that may or may not start in the lung. Healthy people as well as patients with either pulmonary (lung) or nonpulmonary diseases can develop respiratory failure.
The recognition of respiratory failure as a life-threatening problem led to the development of the concept of the intensive care unit (ICU) in modern hospitals. ICU personnel and equipment support vital functions to give patients their best chance for recovery. Today's sophisticated ICU facilities with their novel mechanical life support devices evolved as doctors and scientists learned more and more about the causes of respiratory failure and how to treat it.
This fact book is a brief overview of the unique changes in lung function that are typical of respiratory failure and the widely different medical conditions that can cause those changes. It also discusses the methods that are used to restore normal respiration and prolong life, and the related dilemma of deciding if and when to withdraw or withhold life support from a hopelessly sick patient.
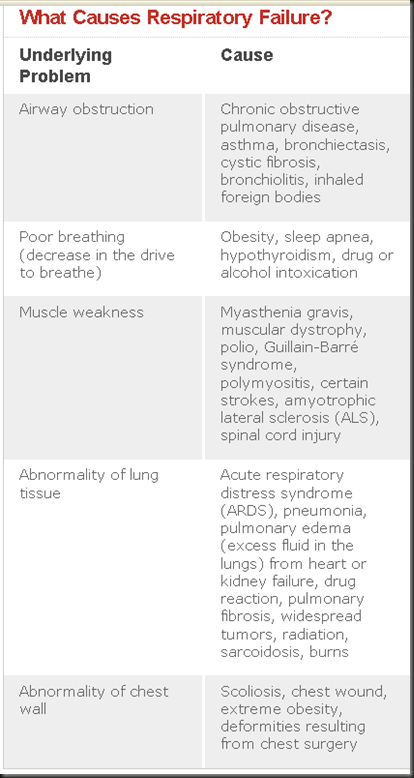
Many different medical conditions can lead to respiratory failure. Listed below are a few examples of people who may develop respiratory failure.
- A patient with a long history of asthma, emphysema, or chronic obstructive lung disease
- A patient who is undergoing major surgery in the abdomen, heart, or lung
- A person who has taken an overdose of sleeping pills or certain depressant drugs
- A premature baby who weighs less than 3 pounds
- A baby with bronchopulmonary dysplasia
- A patient suffering from AIDS
- A person who has received multiple physical injuries
- A person who has suffered extensive burns
- A person who has bled extensively from a gunshot wound
- A person who has almost drowned
- A patient with severe heart failure
- A patient with severe infections
- A person who is extremely obese
Breathing and Respiratory Failure
The term, "respiratory failure," is used when the lungs are unable to perform their basic task - gas exchange. This process involves transfer of oxygen from inhaled air into the blood and of carbon dioxide from the blood into the lungs, with the result that the arterial blood, blood circulating through the body from the heart, has enough oxygen to nourish the tissues.
Gas exchange occurs in tiny air sacs in the lung, called alveoli. When a person breathes in (inspiration), air is brought into the alveoli by the action of the respiratory muscles - the diaphragm, the muscles between the ribs, and the accessory muscles (those between the neck and the chest wall). These are collectively called "the ventilatory apparatus." The activity of the respiratory muscles is controlled by respiratory centers in the brain. The brain's respiratory centers in turn are controlled by chemoreceptors, special cells that are sensitive to the amounts of carbon dioxide or oxygen in the blood. The chemoreceptors that are sensitive to oxygen concentration are located in the large arteries in the neck in the carotid bodies. When they sense a fall in the level of oxygen in the blood, they send messages that stimulate the respiratory center in the brain so that there will be an increase in the rate or depth of breathing.
Whenever any part of the ventilatory apparatus and/or the respiratory centers fails to work properly, the result can be respiratory failure. Both adults and babies can develop respiratory failure. In infants, however, respiratory failure occurs mostly in premature babies whose lungs have not yet fully developed.
Transfer of oxygen of inhaled air into the blood and of waste carbon dioxide of blood into the lungs occurs in the alveolus.
Pathophysiology
When the process of gas exchange is faulty, there is not enough oxygen in the blood (hypoxemia) to fuel the body's metabolic activity. In addition, sometimes there is also an accumulation of carbon dioxide, a waste product of metabolism, in the blood and tissues (hypercapnia). Hypercapnia makes blood more acidic; this condition is called acidemia. Eventually the body tissues become acidic. This condition, called acidosis, injures the body's cells and interferes with the functions of the heart and central nervous system. Ultimately, lack of oxygen in the blood causes death of the cells in the brain and other tissues. If not adequately treated, respiratory failure is fatal.
Types
Hypoxemic Respiratory Failure
When a lung disease causes respiratory failure, gas exchange is reduced because of changes in ventilation (the exchange of air between the lungs and the atmosphere), perfusion (blood flow), or both. Activity of the respiratory muscles is normal. This type of respiratory failure which results from a mismatch between ventilation and perfusion is called hypoxemic respiratory failure. Some of the alveoli get less fresh air than they need for the amount of blood flow, with the net result of a fall in oxygen in the blood. These patients tend to have more difficulty with the transport of oxygen than with removing carbon dioxide. They often overbreathe (hyperventilate) to make up for the low oxygen, and this results in a low CO2 level in the blood (hypocapnia). Hypocapnia makes the blood more basic or alkaline which is also injurious to the cells.Hypercapnic Respiratory Failure
Respiratory failure due to a disease of the muscles used for breathing ("pump or ventilatory apparatus failure") is called hypercapnic respiratory failure. The lungs of these patients are normal. This type of respiratory failure occurs in patients with neuromuscular diseases such as myasthenia gravis, stroke, cerebral palsy, poliomyelitis, amyotrophic lateral sclerosis, muscular dystrophy, postoperative situations limiting ability to take deep breaths, and in depressant drug overdoses. Each of these disorders involves a loss or decrease in neuromuscular function, inefficient breathing and limitation to the flow of air into the lungs. Blood oxygen falls and the carbon dioxide increases because fresh air is not brought into the alveoli in needed amounts. In general, mechanical devices that help move the chest wall help these patients.
Conditions That May Progress To Respiratory Failure
Almost all lung diseases including asthma, chronic obstructive pulmonary disease (COPD), AIDS-related pneumonia, other pneumonias and lung infections, and cystic fibrosis may eventually lead to respiratory failure particularly if the diseases are inadequately treated. These patients find it very hard to breathe and the result is low oxygen and high carbon dioxide blood levels.
People whose normal lungs have been injured, such as from exposure to noxious gases, steam, or heat during a fire, can subsequently go into respiratory failure. Adult respiratory distress syndrome (ARDS), also referred to as acute respiratory distress syndrome, is a form of acute respiratory failure caused by extensive lung injury following a variety of catastrophic events such as shock, severe infection, and burns. ARDS can occur in individuals with or without previous lung disease.
Hyaline membrane disease or respiratory distress syndrome of the newborn (RDS), the most common respiratory illness affecting premature babies, is another kind of respiratory failure. In this condition, the baby's lungs do not have enough surfactant, a substance that makes it possible for air to pass into the alveoli by lowering surface tension and preventing their collapse.
Symptoms Of Respiratory Failure
The clinical features of respiratory failure vary widely in individual patients because so many different conditions can lead to this disorder. There are no physical signs unique to respiratory failure. At extremely low arterial oxygen (PaO2) levels, patients have rapid heart rates, rapid breathing rates, and they are confused, sweaty, and cyanotic (blue). Chronically low arterial oxygen makes patients irritable, and elevated carbon dioxide produces headaches and sleepiness. Difficult, rapid, or labored breathing (dyspnea) is a consistent symptom in the awake patient.The functions of the heart and blood vessels are often severely impaired in patients with respiratory failure. In some cases, chronic hypoxemia produces narrowing of the blood vessels in the lung which, along with the lung damage or the associated treatments, may weaken the heart and the circulatory system. Some of the signs of inadequate circulation are constriction of blood vessels in the skin, cold extremities, and low urine output.
Diagnosis Of Respiratory Failure
It is impossible to estimate the extent of hypoxemia and hypercapnia by observing a patient's signs and symptoms, and mild hypoxemia and hypercapnia may go entirely unnoticed. Blood oxygen must fall markedly before changes in breathing and heart rate occur.
The clinical features of respiratory failure vary widely in individual patients.
The way to diagnose respiratory failure, therefore, is to measure oxygen (PaO2) and carbon dioxide (PaCO2) in the arterial blood. However the levels that indicate respiratory failure are somewhat arbitrary. Depending on age, a PaO2 less than 60 mm Hg or PaCO2 greater than 45 mm Hg generally mean that the patient is in respiratory failure.
Management Of Respiratory Failure
The patient with respiratory failure cannot be adequately treated in the general care areas of the hospital. Therefore, patients in severe respiratory failure are usually treated in the intensive care unit. Current therapy for all forms of respiratory failure attempts, first, to provide support for the heart, lungs, and other affected vital organs; and second, to identify and treat the underlying cause.Since the immediate threat to patients with respiratory failure is due to the inadequate level of oxygen delivered to the tissues, oxygenation is the basic therapy for acute respiratory failure due to lung disease. Oxygen-enriched air is usually given to the patient by nasal prongs, oxygen mask, or by placing an airtube into the trachea (windpipe). Since prolonged high oxygen levels can be toxic, the concentration of oxygen must be carefully controlled for both short- and long-term treatment. Assisted ventilation with mechanical devices may be the first priority for neuromuscular disease patients going into respiratory failure. Additional treatments employ ventilation which helps to keep the lungs inflated at low lung volumes (positive end-expiratory pressure, PEEP), and fluid and nutritional management.
Endotracheal Intubation
Endotracheal intubation involves insertion of a tube into the trachea. It permits delivery of precisely determined amounts of oxygen to the lungs and removal of secretions, and ensures adequate ventilation. Combined with mechanical ventilation, endotracheal intubation is the cornerstone of therapy for respiratory failure.
Mechanical Ventilation
If the patient is tiring despite ongoing therapy, a mechanical ventilator, also called a respirator, is used. The ventilator assists or controls the patient's breathing.Positive End-Expiratory Pressure (PEEP)
Positive end-expiratory pressure is used with mechanical ventilation to keep the air pressure in the trachea at a level that increases the volume of gas remaining in the lung after breathing out (expiration). This keeps the alveoli open, reduces the shunting of blood through the lungs, and improves gas exchange. Most ventilators have a PEEP adjustment.Extracorporeal Membrane Oxygenator (ECMO)
The extracorporeal membrane oxygenator (ECMO) is essentially an artificial lung. It is an appropriately cased artificial membrane which is attached to the patient externally (extracorporeally), through a vein or artery. Although the best substitute for a diseased lung that cannot handle gas exchange adequately is a healthy human lung, such substitution is often not possible. Circulating the patient's blood through the ECMO offers another approach. Gas exchange using ECMO keeps the patient alive while the damaged lungs have a chance to heal.
In 1974, the National Heart, Lung, and Blood Institute (NHLBI) organized a carefully designed clinical trial, to determine the effectiveness of ECMO for patients with acute respiratory distress syndrome. In this study, ECMO appeared to be no more useful than conventional therapy. On the other hand, ECMO seems to be an effective option in some infants with respiratory failure when treatment with mechanical ventilation fails. However ECMO is expensive, is associated with nonrespiratory complications, and is available only in a few specialized centers.
Management of Fluids and Electrolytes
Pulmonary edema, the buildup of abnormal amounts of fluid in the lung tissues, often occurs in respiratory failure. Therefore fluids are carefully managed and monitored to maintain fluid balance and avoid fluid overload which may further worsen gas exchange.Pharmacologic Therapy
Because respiratory failure may be the end result of several different diseases, no single drug therapy is effective in all situations.- Antibiotics help when infections (sepsis) as well as pneumonia are involved in respiratory failure.
- Bronchodilators, for example, theophylline compounds, sympathomimetic agents (albuterol, metaproterenol, isoproterenol), anticholinergics (ipratropium bromide), and corticosteroids, reverse bronchoconstriction and reduce tissue inflammation.
- Other drugs, such as digitalis, improve cardiac output, and drugs which increase blood pressure in shock can improve blood flow to the tissues.
Bronchoscopy
Patients with respiratory failure who have excessive lung secretions are sometimes helped by fiberoptic bronchoscopy, a technique for accessing the interior of the bronchi, the larger air passages of the lungs. The bronchoscope is a flexible tube with a light at the end that is passed through the nose or mouth into the trachea and bronchi. Fluid or tissue can be removed from the bronchi (aspiration), and cells for microscopic examination can be obtained by washing the interior of the larger breathing tubes (lavage). Bronchoscopy is useful for placing or removing endotracheal tubes, removing foreign bodies from the lung, and collecting tissue samples for diagnosis.
Intravenous Nutritional Support
Nutritional supplementation is essential to maintain or restore strength when weakness and loss of muscle mass prevent patients from breathing adequately without ventilatory support. Appropriate nutrients (fats, carbohydrates, and predigested proteins) are fed intravenously for this purpose.Physiotherapy
Physiotherapy includes chest percussion (repeated sharp blows to the chest and back to loosen secretions), suction of airways, and regular changes of body position. It helps drain secretions, maintains alveolar inflation and prevents atelectasis, incomplete expansion of the lung.X-ray Monitoring
X-ray images of the chest help the doctor monitor the progress of lung and heart disease in respiratory failure. The portable chest radiograph taken with an x-ray machine brought to the bedside is often used for this purpose in the intensive care unit.Lung Transplantation
Lung transplantation currently offers the only hope for certain patients with end-stage pulmonary disease. The shortage of suitable donors and the high cost of the procedure continue to be major obstacles that limit its use.Complications of Treatment
Oxygen toxicity, pulmonary embolism (closure of the pulmonary artery or one of its branches by a blood clot or a fat globule), cardiovascular problems, barotrauma (injury to the lung tissue from excessive ventilatory pressure), pneumothorax (air in the pleural space), and gastrointestinal bleeding are some of the complications of treatment. They result from fluid overload, mechanical ventilation, PEEP, and other procedures used in the management of respiratory failure.
Weaning the Patients From Ventilators
The process of returning the patient to unassisted and spontaneous breathing is called weaning. Weaning is a complex process that requires the understanding and cooperation of the patient. It can cause great fatigue and depression in patients because of the slow- and long-term nature of the treatment procedures.Weaning a patient too rapidly or prematurely can be dangerous. Some patients, particularly those who had severe underlying cardiac disease and prolonged episodes of acute illnesses, may require weeks to months to wean. The doctor considers weaning only when the patient is awake, has good nutrition, and is able to cough and breathe deeply.
Discontinuation of Ventilatory Support
The difficult question of whether and when to discontinue life-sustaining mechanical ventilation to the patient who is not responding to any treatment is sometimes faced by the doctor and the family. The legal, ethical, and financial implications of continuing or withholding treatment to the patient in terminal respiratory failure are important issues addressed at family, professional, and government levels. Respecting the rights and wishes of the patient and helping the patient achieve a dignified and peaceful end while continuing to assure care and comfort is a responsibility shared by both the caregivers and the family. The family with a good understanding of respiratory failure in all its dimensions is best equipped to play its part in sharing this responsibility.
More About Some Common Lung Diseases Leading to Or Characterized by Respiratory Failure
Asthma
The hallmarks of asthma are obstruction to air flow and bronchoconstriction, tightening of the muscles in the walls of the bronchi, that is usually relieved by drugs called bronchodilators. Acute asthma attacks that persist, do not respond to bronchodilator therapy, and threaten life are referred to as status asthmaticus. Due to the heavy work of breathing, patients eventually tire and decrease their respiratory efforts. Patients in this condition are prone to develop respiratory failure. Respiratory failure is more common in women with asthma, in patients over 40 years of age, and in patients in whom treatment is delayed, or oral corticosteroid therapy is stopped suddenly.
During an attack of asthma, airways obstruction from mucus secretions and thickened bronchial tissue can lead to severe hypoxemia, hypercapnia, and acidosis. Other potential complications are pneumonia and accumulation of air in pleural spaces. Patients with hypercapnia are at increased risk of death.
In children with asthma, respiratory muscle fatigue and interrupted breathing (apnea) are indications of existing or developing respiratory failure.
Chronic Obstructive Pulmonary Disease (COPD)
COPD patients may develop acute respiratory failure when their chronic airway obstruction is complicated by infections, pulmonary emboli, heart failure, and drug- induced respiratory depression. Influenza often precipitates respiratory failure even without evidence of pneumonia in COPD patients. The hallmark of respiratory failure in COPD is increasing dyspnea and worsening blood gas abnormalities. Depending on the triggering event, various other clinical features may appear. The most dire sign is a decline in the patient's condition associated with PaO2 of less than 50 mm Hg and a PaCO2 greater than 50 mm Hg during air breathing. Uncontrolled administration of oxygen to patients with COPD and acute respiratory failure without therapy directed at reducing the work of breathing can result in further hypercapnia, acidosis, stupor, and coma.
Pneumonia
Patients with very severe pneumonia go into respiratory failure because of lung inflammation and accumulation of fluid that interferes with gas exchange. They breathe hard and become exhausted; their respiratory muscles are unable to keep up the pace. Blood carbon dioxide rises and oxygen in the blood falls further. Sedation, at the time of respiratory stress, may worsen the situation by depression of the brain activity which is needed to keep respiratory muscles working at high levels. This, in turn, decreases the amount of breathing and may promote the development of respiratory failure.
Respiratory Distress Syndrome of the Newborn
One type of respiratory failure in the newborn infant, especially those born prematurely, is commonly referred to as "respiratory distress syndrome." It is also called hyaline membrane disease because of the formation of an abnormal, hyaline (glassy and transparent under the microscope), protein-containing membrane in alveoli. RDS may also occur in full-term babies born to diabetic mothers.
The causes of RDS are complex, but it is believed that the major problem is a poorly developed lung. Surfactant, a unique fat-containing protein necessary to reduce the surface tension in the alveoli of the lung to prevent their collapse, is deficient in RDS babies. The most effective treatment for RDS is the administration of surfactant. Surfactant replacement therapy for RDS, available since 1989, has brought about a 30 percent reduction in death rate for neonatal RDS in the United States (from 89.9 deaths per 100,000 live births in 1989 to 58.3 deaths per 100,000 in 1992). The National Heart, Lung, and Blood Institute (NHLBI) is supporting the development and testing of several different surfactant preparations useful in replacement therapy for RDS.
Adult or Acute Respiratory Distress Syndrome
Acute respiratory failure in adults as a clinical entity was first reported in 1967. Respiratory failure usually occurred following a catastrophic event in individuals with no previous lung disease and who did not respond to ordinary methods of respiratory support. Regardless of the event causing the lung injury, the patients exhibited common signs and symptoms, x-ray findings, and tissue changes. Because many of its features resembled the respiratory distress syndrome of the newborn, RDS, the adult disease was called "ARDS." As with RDS, there is increasing evidence that loss of surfactant function may also be associated with ARDS.
Inhalation of gastric contents (aspiration), pulmonary infections, shock, trauma, burns, extrapulmonary sepsis, inhalation of toxic gases, drug overdose, and near-drowning are some of the different situations that can cause ARDS. An estimated 150,000 cases of ARDS occur yearly in the United States. The estimated mortality rate of ARDS is 50-70 percent.
ARDS is often associated with multiple organ failure (heart, liver, kidneys, and lungs). Patient survival usually depends on the number of organs which fail, the degree and nature of damage, and the age and previous health status of the patient. The incidence of multiple organ failure is particularly high when sepsis or hypotension from loss of blood are the underlying causes of ARDS.
No comments:
Post a Comment