Pleural effusions are accumulations of fluid within the pleural space. They have multiple causes and usually are classified as transudates or exudates. Detection is by physical examination and chest x-ray; thoracentesis and pleural fluid analysis are often required to determine cause. Asymptomatic transudates require no treatment. Symptomatic transudates and almost all exudates require thoracentesis, chest tube drainage, pleurodesis, pleurectomy, or a combination.
Normally, 10 to 20 mL of pleural fluid similar in composition to plasma but lower in protein (< 1.5 g/dL) is spread thinly over visceral and parietal pleurae, facilitating movement between the lung and chest wall. The fluid enters the pleural space from systemic capillaries in the parietal pleurae and exits via parietal pleural stomas and lymphatics. Pleural fluid accumulates when too much fluid enters or too little exits the pleural space.
Etiology
Pleural effusions are usually categorized as transudates or exudates based on laboratory characteristics of the fluid (Mediastinal and Pleural Disorders: Criteria for Identifying Exudative Pleural Effusions). Whether unilateral or bilateral, a transudate can usually be treated without extensive evaluation, whereas the cause of an exudate requires investigation. There are numerous causes (Mediastinal and Pleural Disorders: Causes of Pleural Effusion ).
Transudative effusions are caused by some combination of increased hydrostatic pressure and decreased plasma oncotic pressure. Heart failure is the most common cause, followed by cirrhosis with ascites and hypoalbuminemia, usually from the nephrotic syndrome.
Exudative effusions are caused by local processes leading to increased capillary permeability resulting in exudation of fluid, protein, cells, and other serum constituents. Causes are numerous, the most common being pneumonia, cancer, pulmonary embolism, viral infection, and TB. Yellow nail syndrome is a rare disorder causing chronic exudative pleural effusions, lymphedema, and dystrophic yellow nails, all thought to be the result of impaired lymphatic drainage.
Chylous effusion (chylothorax) is a milky white effusion high in triglycerides caused by traumatic or neoplastic (most often lymphomatous) damage to the thoracic duct. Chylous effusion also occurs with the superior vena cava syndrome.
Chyliform (cholesterol or pseudochylous) effusions resemble chylous effusions but are low in triglycerides and high in cholesterol. Chyliform effusions are thought to be due to release of cholesterol from lysed RBCs and neutrophils in long-standing effusions when absorption is blocked by the thickened pleura.
Hemothorax is bloody fluid (pleural fluid Hct > 50% peripheral Hct) in the pleural space due to trauma or, rarely, as a result of coagulopathy or after rupture of a major blood vessel, such as the aorta or pulmonary artery.
Empyema is pus in the pleural space. It can occur as a complication of pneumonia, thoracotomy, abscesses (lung, hepatic, or subdiaphragmatic), or penetrating trauma with secondary infection. Empyema necessitatis is soft-tissue extension of empyema leading to chest wall infection and external drainage.
Trapped lung is lung encased by a fibrous peel caused by empyema or tumor. Because the lung cannot expand, the pleural pressure becomes more negative than normal, increasing transudation of fluid from parietal pleural capillaries. The fluid characteristically is borderline between a transudate and an exudate, ie, the biochemical values are within 15% of the cutoff levels for Light's criteria (see Table 2: Mediastinal and Pleural Disorders: Criteria for Identifying Exudative Pleural Effusions).
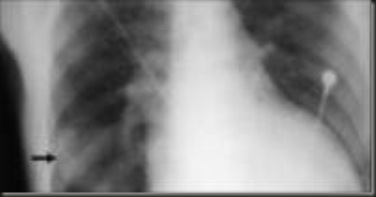
Iatrogenic effusions can be caused by migration or misplacement of a feeding tube into the trachea or perforation of the superior vena cava by a central venous catheter, leading to infusion of tube feedings or IV solution into the pleural space.
Effusions with no obvious cause are often due to occult pulmonary emboli, TB, or cancer. Etiology is unknown for about 15% of effusions even after extensive study; many of these effusions are thought to be due to viral infection.
Some pleural effusions are asymptomatic and are discovered incidentally on physical examination or chest x-ray. Many cause dyspnea, pleuritic chest pain, or both. Pleuritic chest pain, a vague discomfort or sharp pain that worsens on inspiration, indicates inflammation of the parietal pleura. Pain is usually felt over the inflamed site, but referred pain is possible. The posterior and peripheral portions of the diaphragmatic pleura are supplied by the lower 6 intercostal nerves, and irritation there may cause pain in the lower chest wall or abdomen that may simulate intra-abdominal disease. Irritation of the central portion of the diaphragmatic pleura, innervated by the phrenic nerves, causes pain referred to the neck and shoulder.
Physical examination reveals absent tactile fremitus, dullness to percussion, and decreased breath sounds on the side of the effusion. These findings can also be produced by pleural thickening. With large-volume effusions, respiration is usually rapid and shallow. A pleural friction rub, although infrequent, is the classic physical sign. The friction rub varies from a few intermittent sounds that may simulate crackles to a fully developed harsh grating, creaking, or leathery sound synchronous with respiration, heard on inspiration and expiration. Friction sounds adjacent to the heart (pleuropericardial rub) may vary with the heartbeat and may be confused with the friction rub of pericarditis. Pericardial rub is best heard over the left border of the sternum in the 3rd and 4th intercostal spaces, is characteristically a to-and-fro sound synchronous with the heartbeat, and is not influenced significantly by respiration. Sensitivity and specificity of the physical examination for detecting effusion are probably low.
Pleural effusion is suspected in patients with pleuritic pain, unexplained dyspnea, or suggestive signs. Diagnostic tests are indicated to document the presence of pleural fluid and to determine its cause (see Fig. 2: Mediastinal and Pleural Disorders: Diagnosis of Pleural Effusion).
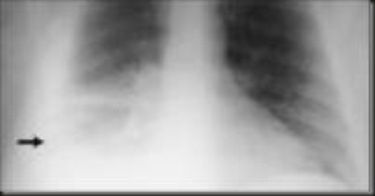
Presence of effusion: Chest x-ray is the first test done to confirm the presence of pleural fluid. The lateral upright chest x-ray should be examined when a pleural effusion is suspected. In an upright film, 75 mL of fluid blunts the posterior costophrenic angle. Blunting of the lateral costophrenic angle usually requires about 175 mL but may take as much as 500 mL. Larger pleural effusions opacify portions of the hemithorax and may cause mediastinal shift; effusions > 4 L may cause complete opacification of the hemithorax and mediastinal shift to the contralateral side.
Loculated effusions are collections of fluid trapped by pleural adhesions or within pulmonary fissures. Lateral decubitus x-rays, chest CT, or ultrasound should be done if it is unclear whether an x-ray density represents fluid or parenchymal infiltrates or whether suspected fluid is loculated or free-flowing; these tests are more sensitive than upright films and can detect fluid volumes < 10 mL. Loculated effusions, particularly those in the horizontal or oblique fissure, can be confused with a solid pulmonary mass (pseudotumor). They may change shape and size with changes in the patient's position and amount of pleural fluid.
CT scan is not routinely indicated but is valuable for evaluating the underlying lung parenchyma for infiltrates or masses when the lung is obscured by the effusion or when the detail on chest x-rays is insufficient and for distinguishing loculated fluid from solid mass.
Cause of effusion: Thoracentesis should be done on almost all patients who have pleural fluid that is ≥ 10 mm in thickness on CT, ultrasound, or lateral decubitus x-ray and that is new or of uncertain etiology. In general, the only patients who do not require thoracentesis are those who have heart failure with symmetric pleural effusions and no chest pain or fever; in these patients, diuresis can be tried, and thoracentesis avoided unless effusions persist for ≥ 3 days.
Despite common practice, chest x-ray need not be repeated after thoracentesis unless patients develop symptoms suggestive of pneumothorax (dyspnea or chest pain) or unless there is reason to suspect that air may have entered the pleural space during the procedure. Thoracentesis and subsequent pleural fluid analysis often are not necessary for pleural effusions that are chronic, have a known cause, and cause no symptoms.
Ultrasonography is helpful for identifying the site for thoracentesis when the amount of pleural fluid is small, the fluid is loculated, or blind thoracentesis is unsuccessful.
Pleural fluid analysis is done to diagnose the cause of pleural effusion. Analysis begins with visual inspection, which can
- Distinguish bloody and chylous (or chyliform) from other effusions
- Identify purulent effusions strongly suggestive of empyema
- Identify viscous fluid, which is characteristic of some mesotheliomas
Fluid should always be sent for total protein, LDH, cell count and cell differential, Gram stain, and aerobic and anaerobic bacterial cultures. Other tests (glucose, cytology, TB fluid markers [ adenosine Some Trade Names
ADENOCARD
deaminase or interferon-γ], amylase, mycobacterial, and fungal stains and cultures) are used in appropriate clinical settings.
Fluid chemistries help distinguish transudates from exudates; multiple criteria exist, not one of which perfectly discriminates between the two. When Light's criteria are used, the serum LDH and total protein for comparison with pleural fluid should be obtained as close as possible to the time of thoracentesis. Light's criteria correctly identify almost all exudates but misidentify about 20% of transudates as exudates. If transudative effusion is suspected (eg, due to heart failure or cirrhosis) and none of the biochemical measurements are > 15% above the cutoff levels for Light's criteria, then the difference between the serum and the pleural fluid protein is measured. If the difference is > 3.1 g/dL, then the patient probably has a transudative effusion.
If the diagnosis remains unclear after pleural fluid analysis, a helical CT scan is indicated to look for pulmonary emboli, pulmonary infiltrates, or mediastinal lesions. Findings of pulmonary emboli indicate the need for long-term anticoagulation; parenchymal infiltrates, the need for bronchoscopy; and mediastinal lesions, the need for transthoracic needle aspiration or mediastinoscopy. However, helical CT requires patients to hold their breath for ≥ 24 sec, and not all patients can comply. If helical CT is unrevealing, observation is the best course unless the patient has a history of cancer, weight loss, persistent fever, or other findings suggestive of cancer or TB, in which case thoracoscopy may be indicated. Needle biopsy of the pleura can be done when thoracoscopy is unavailable. When thoracoscopy is unrevealing, an open thoracotomy must sometimes be done. Most patients with exudative effusions should have a PPD placed with controls, but TB can neither be diagnosed if the PPD result is positive nor definitively excluded if it is negative, so pleural biopsy is generally needed.
Treatment
- Symptoms and underlying disorder treated
- Drainage of some symptomatic effusions
- Other treatments for parapneumonic and malignant effusions
The effusion itself generally does not require treatment if it is asymptomatic when the underlying disorder is treated, because many effusions resorb spontaneously, especially those due to uncomplicated pneumonias, pulmonary embolism, and surgery. Pleuritic pain can usually be managed with NSAIDS or other oral analgesics. At times a short course of oral opioids is required.
Thoracentesis is sufficient treatment for many symptomatic effusions and can be repeated for effusions that reaccumulate. Removal of fluid can be continued until the patient develops chest tightness, chest pain, or severe coughing.
Effusions that are chronic, recurrent, and causing symptoms can be treated with pleurodesis or by intermittent drainage with an indwelling catheter). Effusions caused by pneumonia and cancer may require additional specific measures.
Parapneumonic effusion and empyema: In the presence of adverse prognostic factors (pH < 7.20, glucose < 60 mg/dL, positive Gram stain or culture, loculations), the effusion should be completely drained via thoracentesis or tube thoracostomy. If complete drainage is impossible, a thrombolytic (fibrinolytic) drug (eg, urokinase 100,000 units or tissue plasminogen activator 10 mg in 100 mL saline solution) can be administered intrapleurally, but the effectiveness of this intervention is unproved. If attempts at drainage are unsuccessful, thoracoscopy should be done to lyse adhesions, and remove fibrous tissue coating the lung to allow the lung to expand. If thoracoscopy is unsuccessful, thoracotomy with surgical decortication (eg, removal of scar, clot, or fibrous membrane surrounding the lung) is necessary.
Malignant pleural effusion: If dyspnea caused by malignant pleural effusion is relieved by thoracentesis but fluid reaccumulates (with dyspnea), chronic (intermittent) drainage or pleurodesis is indicated. Asymptomatic effusions and those for which thoracentesis does not relieve dyspnea do not require additional procedures.
Indwelling catheter drainage is the preferred approach for ambulatory patients, because hospitalization is not necessary for catheter insertion and the pleural fluid can be drained intermittently into vacuum bottles. Pleurodesis is created by instilling a sclerosing agent into the pleural space to fuse the visceral and parietal pleura and eliminate the space. The most effective and commonly used sclerosing agents are talc, doxycycline Some Trade Names
PERIOSTAT
VIBRAMYCIN
, and bleomycin Some Trade Names
BLENOXANE
delivered via chest tube or thoracoscopy. Pleurodesis is contraindicated if the mediastinum has shifted toward the side of the effusion or if the lung does not expand after a chest tube is inserted.
Shunting of pleural fluid to the peritoneum (pleuroperitoneal shunt) is useful for patients with malignant effusion in whom pleurodesis is unsuccessful and in patients who have trapped lung.


No comments:
Post a Comment